Table of Contents >> Show >> Hide
- Before You Treat It, Name It: What “Deep Cough” Usually Means
- Way #1: Thin the Mucus (So Your Cough Can Actually Finish the Job)
- Way #2: Soothe the Irritation (Especially if Your Cough Is Dry, Painful, or Nighttime-Loud)
- Way #3: Treat the Triggers That Keep a Deep Cough Alive
- Way #4: Know When to Get Medical Backup (Because Some Deep Coughs Aren’t a DIY Project)
- A Simple 48-Hour Deep Cough Game Plan
- FAQs About Deep Cough Relief
- Experience Section: What People Commonly Try (and What Tends to Help)
- Scenario 1: The Classic Chest Cold Cough (a.k.a. “Why am I still coughing?!”)
- Scenario 2: The Postnasal Drip Night Cough (the “I’m fine all day, then bedtime happens” problem)
- Scenario 3: The Reflux Cough (the “I don’t even have heartburn!” plot twist)
- Scenario 4: The “It’s Not Getting Better” Cough (the one that needs a professional opinion)
- Conclusion
A “deep cough” is the kind that feels like it’s coming from your chest, not your throatlike your lungs are trying to
return an item without a receipt. It can be loud, stubborn, and annoying enough to make you consider communicating
only through interpretive dance.
The good news: most deep coughs are treatable at home, especially if they’re tied to a viral cold or chest cold.
The better news: you don’t have to “tough it out” with zero strategy. Below are four practical, evidence-based ways
to calm a deep cough and help your body clear what it needs to clear.
Quick note: This article is for general education, not personal medical advice. If you have severe symptoms,
trouble breathing, or a cough that won’t quit, get evaluated by a clinician.
Before You Treat It, Name It: What “Deep Cough” Usually Means
“Deep cough” is more of a feeling than a diagnosis. Most often, it’s one of these:
- Wet/productive cough: you’re coughing up mucus (phlegm). Your body is trying to move sticky stuff out.
-
Dry cough: no mucus, but the cough still feels chestyoften from irritation, inflammation, or triggers
like postnasal drip, asthma, or reflux.
A deep cough from a cold or acute bronchitis commonly improves over days to a couple of weeks, but it can linger.
If you’re dealing with a persistent cough, the best approach is to treat the symptom and the likely cause.
That’s where the four methods below come in.
Way #1: Thin the Mucus (So Your Cough Can Actually Finish the Job)
If your deep cough sounds “wet,” rattly, or gurgly, mucus is probably part of the problem. In that case, the goal
isn’t to silence the cough at all costsit’s to make the cough more effective and less exhausting by loosening what’s
stuck.
Hydrate like you mean it
Mucus gets thicker when you’re dehydrated. Thick mucus is the clingy ex who keeps texting at 2 a.m.: hard to ignore and
weirdly committed. Water, warm tea, broth, and warm lemon water can help keep secretions thinner and easier to move.
Practical tip: if your urine is dark yellow, treat hydration as part of your cough plannot a “nice-to-have.”
Aim for steady sipping throughout the day instead of chugging a gallon at bedtime (unless you enjoy nighttime bathroom
cardio).
Add moisture to the airways (steam + humidifier)
Moist air can make a deep chest cough feel less harsh by soothing irritated airways and helping loosen mucus. Two simple
options:
- Steam: a warm shower or sitting in a steamy bathroom for 10–15 minutes.
- Cool-mist humidifier: especially helpful at night when coughing gets dramatic.
Humidifier reality check: humidifiers help, but a dirty humidifier can also turn into a tiny swamp
machine. Keep humidity moderate and clean the unit regularly. Use the device safelyespecially around kids.
Consider an expectorant for chest congestion (read: guaifenesin)
If chest congestion is making your cough feel deep and heavy, an over-the-counter expectorant with
guaifenesin can help by thinning and loosening mucus so you can cough it up more easily.
It won’t “turn off” coughingit’s meant to make coughing useful.
Smart use: expectorants work best when you’re also drinking fluids. Also, check labels: many products
combine multiple ingredients (decongestants, antihistamines, cough suppressants). If you’re unsure what you’re taking,
ask a pharmacistthis is literally their Super Bowl.
Way #2: Soothe the Irritation (Especially if Your Cough Is Dry, Painful, or Nighttime-Loud)
Sometimes the cough is less about mucus and more about irritated, over-sensitive airways. That’s when your body coughs
because the air feels “wrong” (dry, cold, dusty, perfumed, spicybasically the world is offending your lungs).
Your strategy here is to calm the tissue and reduce the cough reflexwithout doing anything sketchy.
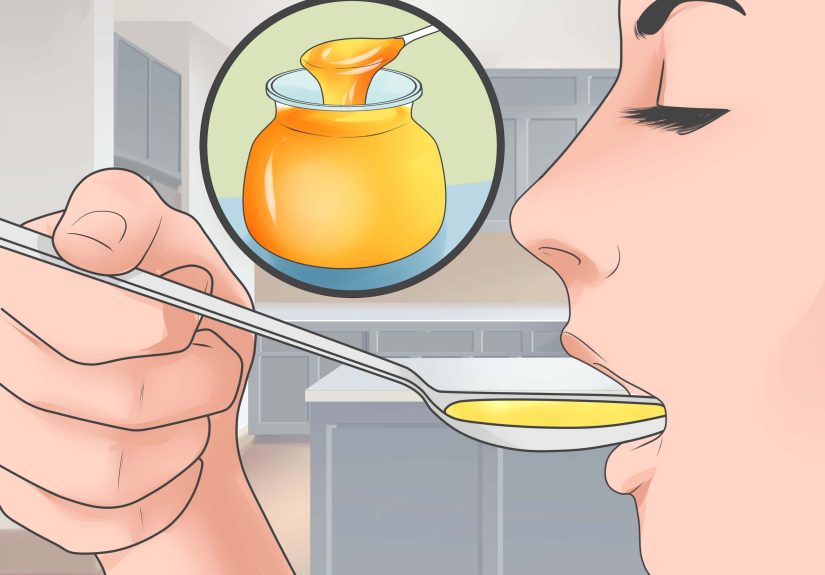
Honey: small spoon, big energy
Honey can coat the throat and reduce coughingespecially at night. It’s often used in warm tea or warm water, but a
teaspoon straight-up can work too.
Important safety note: never give honey to children under 1 year old.
Lozenges, warm liquids, and “throat-first aid”
If your deep cough is triggering a sore throat, treat the throat as part of the cough. Cough drops/lozenges can soothe
irritation and reduce the urge to cough. Warm liquids can also help (bonus points for not tasting like a chemistry set).
If your throat feels scratchy, a saltwater gargle is old-school for a reason. It’s simple, cheap, and doesn’t require
learning a new supplement influencer’s name.
When a cough suppressant makes sense (and when it doesn’t)
If your cough is keeping you from sleeping or causing chest soreness from nonstop coughing, an OTC cough suppressant
(often dextromethorphan) may reduce the cough reflex for short-term relief.
- Better fit: dry cough, tickle-cough, or nighttime cough when mucus isn’t the main issue.
-
Use caution: if you’re coughing up a lot of mucus, suppressing the cough too much may make it harder to
clear secretions.
Always follow label directions, especially with combination products (it’s easy to accidentally double-dose
the same ingredient across multiple “cold & cough” items).
Way #3: Treat the Triggers That Keep a Deep Cough Alive
Here’s the rude truth: a deep cough can linger because something keeps poking the “cough button.”
If you don’t address the trigger, you’ll keep coughing even after the original cold packed its bags.
The big repeat offenders are postnasal drip, acid reflux (GERD), and irritants.
Trigger A: Postnasal drip (upper airway cough syndrome)
When mucus drips down the back of your throat, it can irritate your airway and create a cough that feels deepespecially
when you lie down.
- Try saline: a saline nasal spray or rinse can thin and clear mucus.
- Consider allergy support: if seasonal allergies are involved, targeted allergy treatment may help.
- Sleep angled: elevating your head can reduce nighttime drip and coughing fits.
Common experience: people often notice they’re clearing their throat constantly or feeling a “drip” even
when their nose isn’t running much. That’s your clue.
Trigger B: Acid reflux (GERD) that shows up as a cough
Reflux isn’t always obvious heartburn. For some people, stomach acid irritates the upper airway and contributes to a
chronic, stubborn cough.
You can test-drive reflux-friendly habits for a couple of weeks:
- Don’t eat late: stop food (and most drinks besides water) 2–3 hours before bed.
- Elevate your head: use a wedge pillow or raise the head of your bed.
- Watch triggers: alcohol, peppermint, spicy foods, and very fatty meals commonly worsen reflux.
If your cough is worse after meals, worse at night, or paired with hoarseness, reflux is worth considering. If you’re
not improving, talk with a clinicianreflux management can be more nuanced than “just take something and pray.”
Trigger C: Irritants (smoke, dust, fragrances, dry air, and “why is that candle so aggressive?”)
Airway irritation can keep a deep cough going even after the infection is gone. If you smoke, vaping or cigarettes can
prolong inflammation and coughing. Secondhand smoke also matters.
Low-effort wins: avoid smoky rooms, skip strong fragrances, crack a window when air feels stale, and keep
humidity comfortable (not tropical rainforest levels).
Support the basics: rest and gentle movement
Rest helps recovery. Light movement (like an easy walk) can sometimes help loosen chest congestion, but if you’re
wheezing, feverish, or getting short of breath, scale back and get evaluated.
Way #4: Know When to Get Medical Backup (Because Some Deep Coughs Aren’t a DIY Project)
Home remedies can be greatbut they’re not a magic spell. A deep cough can signal bronchitis, asthma, pneumonia, medication
side effects, or other issues. The fastest way to “get rid of it” is sometimes to identify the underlying cause and treat
that directly.
Red flags: don’t wait these out
- Trouble breathing, shortness of breath, or worsening wheezing
- Coughing up blood (or rust-colored mucus)
- Fever that’s high, persistent, or returns after you started improving
- Chest pain that feels severe, tight, or not just “my ribs are tired from coughing”
- Fainting, confusion, significant weakness, or dehydration
- Unexplained weight loss or swelling in the legs/ankles
How long is “too long” for a deep cough?
A cough from a typical chest cold often improves within a few weeks, but timing matters:
- Over 3 weeks and not improving: time to check in.
- Over 8 weeks (adults): this is considered chronic and deserves a workup.
- Kids: prolonged cough in children should be discussed with a pediatric clinician sooner.
Why antibiotics usually aren’t the answer (and when they are)
Many deep coughs come from viral infections, and antibiotics don’t treat viruses. Taking antibiotics “just in case”
can cause side effects and contributes to antibiotic resistance. However, antibiotics may be appropriate if a clinician
diagnoses certain bacterial infections (like pneumonia or pertussis/whooping cough) or other complications.
What a clinician might look for (so you can show up prepared)
If your cough won’t leave, a clinician may ask about:
- Asthma symptoms (including cough-variant asthma)
- Allergies/postnasal drip patterns
- Reflux symptoms or nighttime cough
- Smoking/vaping exposure
- Medication side effects (some blood pressure meds can trigger cough)
- Whether you need tests like a chest X-ray or breathing tests
Pro tip: bring a mini timeline: when it started, what helps, what worsens it, and what you’ve tried.
It turns your appointment from “mystery novel” into “clear plot summary.”
A Simple 48-Hour Deep Cough Game Plan
If you like structure (or your cough has turned you into a sleep-deprived goblin who needs a checklist), try this:
Morning
- Warm drink + water (start thinning mucus early)
- Steam (shower) or humidifier time
- Saline nasal spray/rinse if you feel drip or stuffiness
Daytime
- Steady fluids every hour
- Avoid smoke/fragrance triggers
- Consider guaifenesin if chest congestion is significant (follow label directions)
- Light movement if you feel up to it
Night
- Honey (if age-appropriate) or warm tea
- Humidifier on a clean setting
- Elevate your head if postnasal drip or reflux seems likely
- Cough suppressant only if the cough is dry and ruining sleep (follow labels carefully)
FAQs About Deep Cough Relief
What if my cough is dry but still feels “deep”?
That can happen with airway irritation, asthma, postnasal drip, or reflux. Try the soothing steps (honey, humidifier,
lozenges) and address triggers (drip/reflux/irritants). If it persists beyond a few weeks or you have red flags, get checked.
Should I try to stop the cough completely?
Not always. If you’re producing mucus, coughing helps clear it. The goal is to make your cough more productive and less
constantthen use suppression strategically (like at night) if needed.
What if the cough keeps coming back?
Recurrent deep cough can suggest triggers like allergies, asthma, reflux, smoking exposure, or repeated infections.
That’s a good reason to see a clinician for a targeted plan rather than cycling through random cough syrups forever.
Experience Section: What People Commonly Try (and What Tends to Help)
Let’s talk real lifebecause cough advice sounds tidy until you’re awake at 2:17 a.m., bargaining with the universe
like, “If I can just stop coughing for five minutes, I promise I’ll finally clean the humidifier.”
Below are three common “deep cough” storylines people report, plus what usually makes the biggest difference. Think of
these as composite scenariosnot medical diagnoses, but practical patterns.
Scenario 1: The Classic Chest Cold Cough (a.k.a. “Why am I still coughing?!”)
This often starts as a normal coldrunny nose, sore throat, mild fatigue. Then, just when you think you’re improving,
the cough moves into your chest and sticks around. People describe it as heavy, sometimes wet, and annoyingly persistent.
What tends to help most: hydration + humidified air + patience with a plan. When folks commit to steady
fluids (not just one heroic bottle of water), use steam or a cool-mist humidifier at night, and consider an expectorant
if mucus is thick, the cough often becomes less violent and more productive. The “win” isn’t instant silenceit’s fewer
coughing fits and better sleep.
Scenario 2: The Postnasal Drip Night Cough (the “I’m fine all day, then bedtime happens” problem)
People with this pattern often say: “I’m okay during the day, but I cough as soon as I lie down.” Sometimes there’s a
tickle in the throat, frequent throat-clearing, or a feeling like mucus is parked in the back of the throat.
What tends to help most: saline + elevation + consistency. A saline spray or rinse can reduce drip,
and sleeping with the head slightly elevated can stop the nighttime waterfall effect. If allergies are part of it,
targeted allergy control can be a game-changer. People often notice improvement when they stop treating it like “a chest
cough only” and start treating the nose and throat as part of the system.
Scenario 3: The Reflux Cough (the “I don’t even have heartburn!” plot twist)
This one sneaks up. The cough may be dry, stubborn, and worse at night or after meals. People sometimes report hoarseness
or a “lump in the throat” sensation. The surprising part is that reflux can show up as coughing even when classic heartburn
isn’t obvious.
What tends to help most: timing and positioning. People often see improvement when they stop eating a couple
of hours before bed, elevate the head of the bed, and reduce common triggers like alcohol or late-night spicy meals.
It’s not glamorous, but neither is coughing through your entire streaming queue.
Scenario 4: The “It’s Not Getting Better” Cough (the one that needs a professional opinion)
Sometimes the deep cough is trying to tell you something importantlike asthma, pneumonia, medication side effects, or
another condition that needs targeted treatment. People often realize it’s time to get checked when the cough lasts past a
few weeks, keeps recurring, or comes with shortness of breath, fever, or chest pain.
What tends to help most: bringing details to the appointment. People who track a few specificshow long it’s
lasted, whether it’s wet or dry, what triggers it (cold air, exercise, lying down), and what they’ve already triedoften
get a faster, clearer plan. And yes: sometimes the best cough remedy is simply the correct diagnosis.
Bottom line: people get the best results when they stop chasing the cough like it’s a whack-a-mole game and instead combine
(1) mucus-thinning, (2) airway soothing, (3) trigger control, and (4) smart escalation when needed.