Table of Contents >> Show >> Hide
- Why kidney disease matters (even when you feel fine)
- Ozempic vs Wegovy: same ingredient, different “day jobs”
- What the science says: why semaglutide is being linked to kidney protection
- How semaglutide might help the kidneys (without the magic wand)
- Who may benefit most (and who needs extra caution)
- Practical takeaways if you’re thinking about semaglutide for kidney risk
- What we still don’t know (yet)
- Bottom line
- Experiences related to “Ozempic, Wegovy May Help Reduce Kidney Disease Risk” (Real-world perspective)
- Experience #1: “My labs became a storyline, not a surprise plot twist”
- Experience #2: “The nausea was real, but so was the hydration strategy”
- Experience #3: “Weight loss made my blood pressure meds feel… too strong”
- Experience #4: “I expected a miracle. I got momentum (and that’s actually better).”
- Experience #5: “The best results came from teamwork, not from one pen”
Your kidneys are basically the ultimate “quiet coworkers.” They filter waste, balance fluids, help control blood pressure,
and do a dozen other jobs without asking for credit. The problem? Chronic kidney disease (CKD) is also quietuntil it isn’t.
That’s why recent evidence around semaglutide (the active ingredient in Ozempic and Wegovy) has people paying attention:
these GLP-1 medicines may do more than lower blood sugar or support weight lossthey may also help protect kidney health.
The headline sounds almost too good: a medication known for appetite changes and smaller portions might also help reduce
the risk of kidney disease progression. But this isn’t just internet hype or a “my cousin’s neighbor’s dog walker” story.
Large clinical trials and updated prescribing information now connect semaglutide to meaningful kidney outcomes in specific
patient groups. The key is understanding what the evidence actually shows, who it applies to, and what “kidney protection”
really means in real life.
Why kidney disease matters (even when you feel fine)
CKD is common in the U.S., and it often flies under the radar. Many people don’t have symptoms in early stages, which is
why CKD is sometimes described as a “silent” condition. Screening typically relies on two routine measurements:
- eGFR (estimated glomerular filtration rate): a blood-test estimate of how well your kidneys filter.
- UACR (urine albumin-to-creatinine ratio): a urine test that checks for albumin leakage, a sign of kidney damage.
In plain English: eGFR helps tell you how well the kidneys are filtering, and UACR helps tell you whether the kidney’s
“filter” is getting leaky. In many clinical settings, a UACR above 30 mg/g suggests albuminuria and higher kidney risk, even
if you feel totally normal.
Diabetes and high blood pressure are major drivers of CKD in the United States. Obesity can also raise kidney risk directly
and indirectlyby worsening insulin resistance, blood pressure, inflammation, and heart health. So when a medication improves
blood sugar, weight, and cardiovascular outcomes, it’s not a huge leap to ask: could it also help the kidneys?
Ozempic vs Wegovy: same ingredient, different “day jobs”
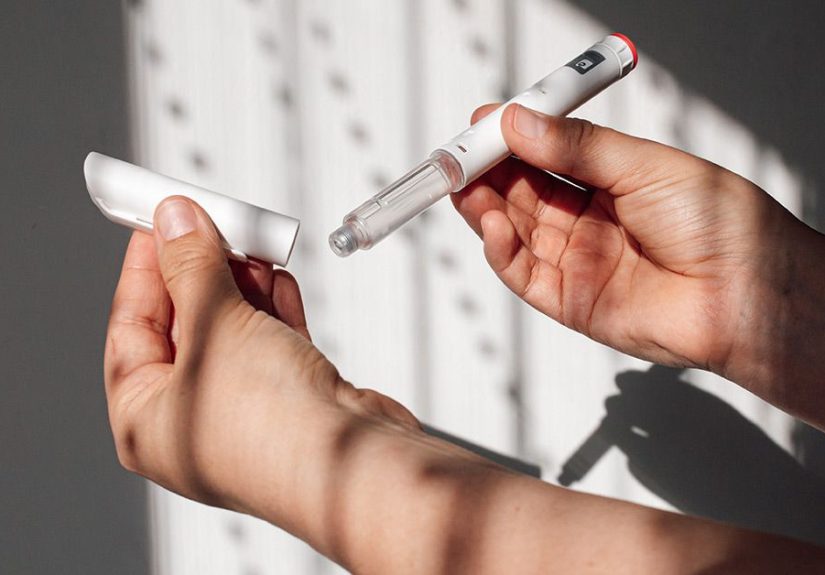
Ozempic and Wegovy both contain semaglutide, a GLP-1 receptor agonist. Think of GLP-1 as a hormone-like signal that
helps the body manage blood sugar and appetite. Semaglutide can:
- Increase insulin release when blood sugar is high
- Reduce glucagon (a hormone that raises blood sugar)
- Slow stomach emptying (which can help with fullness)
- Reduce appetite and support weight loss
The differences are mainly about indications and dosing:
- Ozempic is primarily used for type 2 diabetes (and certain cardiovascular and kidney-risk reductions in defined groups).
- Wegovy is used for chronic weight management and also for reducing major cardiovascular events in certain adults with overweight/obesity.
Here’s the important nuance for kidney health: Ozempic now has an FDA-recognized role in reducing certain kidney-related risks
in adults with type 2 diabetes and chronic kidney disease. Wegovy’s kidney story is more “strong evidence is emerging,”
rather than “this is the official labeled kidney indication for everyone.”
What the science says: why semaglutide is being linked to kidney protection
When people say Ozempic or Wegovy may reduce kidney disease risk, they’re usually pointing to a few key outcomes:
slower decline in eGFR, reduced albumin in the urine, fewer events like end-stage kidney disease, and fewer serious kidney-related
complications over time. Two major pieces of evidence have shaped the conversation.
1) The FLOW trial: semaglutide in people with type 2 diabetes and CKD
The FLOW trial was designed specifically to answer a kidney question: does semaglutide improve “hard” kidney outcomes in people who
already have type 2 diabetes and chronic kidney disease? This wasn’t a tiny study with wishful thinkingit was a large, randomized,
placebo-controlled trial with years of follow-up.
In the FLOW results (published in a major medical journal), semaglutide reduced the risk of clinically important kidney outcomes
compared with placebo. In practical terms, the semaglutide group experienced fewer events tied to kidney disease progression and fewer
serious outcomes over time. The trial also reported cardiovascular benefit, which matters because CKD and heart disease are frequent
(unpleasant) roommates.
This is the kind of data that moves beyond “promising” and into “practice-changing for the right patients.” It also helps explain why
regulatory language about kidney outcomes has expanded for Ozempic in adults with type 2 diabetes and CKD.
2) SELECT kidney outcomes analysis: semaglutide 2.4 mg in people with overweight/obesity (without diabetes)
SELECT is widely known for showing cardiovascular risk reduction with semaglutide 2.4 mg in adults with overweight/obesity and established
cardiovascular disease who did not have diabetes. But a pre-specified kidney outcomes analysis added another layer: semaglutide was associated
with fewer kidney-related events and improved kidney markers such as albuminuria and the rate of eGFR decline.
Why does this matter? Because it suggests kidney benefits may not be limited only to glucose control. Weight reduction, blood pressure changes,
improved inflammation profiles, and direct kidney effects may also play a role. That said, it’s crucial to interpret this appropriately:
SELECT’s primary endpoint was cardiovascular, and kidney outcomeswhile carefully assessedsit in the “very encouraging evidence” category rather than
a blanket promise that everyone will avoid CKD.
3) The bigger picture: GLP-1 drugs and kidney outcomes as a class
Semaglutide isn’t the first GLP-1 medicine to show kidney-related signals. Earlier trials of GLP-1 receptor agonists in type 2 diabetes often showed
reductions in albuminuria (a key risk marker) and some improvement in composite kidney endpoints, though the strongest “hard kidney outcome” evidence
has become clearer more recently with dedicated trials and larger analyses.
Meta-analyses pooling multiple GLP-1 trials suggest a meaningful reduction in clinically important kidney events. That doesn’t mean GLP-1 medicines are
a replacement for established kidney-protective therapiesbut it does reinforce that the kidney benefits appear consistent enough to take seriously.
How semaglutide might help the kidneys (without the magic wand)
Kidneys are sensitive to metabolic stress. Semaglutide can affect several kidney-relevant pathways at oncesome indirectly (through overall health improvements),
and some possibly directly (through kidney and vascular biology). Potential mechanisms include:
- Better blood sugar control, which reduces long-term damage to kidney filtration structures in diabetes.
- Weight loss, which can lower kidney workload and improve blood pressure and metabolic inflammation.
- Lower blood pressure (often modest but meaningful), reducing pressure inside kidney filtering units.
- Improved cardiovascular health, which supports kidney perfusion and reduces cardiorenal stress.
- Reduced albuminuria, which is both a marker and a mediator of ongoing kidney injury.
The most honest summary is this: semaglutide appears to shift several risk factors in a kidney-friendly direction, and in certain high-risk groups,
trials show that translates into fewer serious kidney outcomes. That’s not “kidney disease cured,” but it is “kidney disease slowed,” which is often
the real goal in CKD care.
Who may benefit most (and who needs extra caution)
People who may see the strongest kidney-related benefit
- Adults with type 2 diabetes and chronic kidney disease, especially those at risk of faster progression
- Adults with overweight/obesity and cardiovascular disease, where evidence suggests kidney markers and outcomes may improve
- People with albuminuria (elevated UACR), where reductions in urine albumin may signal lower progression risk
People who should be especially careful
Even though semaglutide can support kidney health over time, it can also trigger situations that temporarily stress the kidneysespecially early on.
The most common culprit is dehydration from gastrointestinal side effects.
-
Risk of acute kidney injury due to volume depletion: nausea, vomiting, and diarrhea can reduce fluid intake and cause dehydration.
If you already have CKD, that dehydration can be a bigger deal. - People prone to dehydration: older adults, those on diuretics (“water pills”), and people who struggle with adequate fluid intake.
- Those with severe GI symptoms: if you can’t keep fluids down, kidney function should be monitored and the prescribing clinician should be notified.
Also worth noting: Ozempic’s prescribing information indicates no dose adjustment is generally recommended for renal impairment, based on pharmacokinetics.
But “no dose adjustment” is not the same as “no monitoring needed.” Anyone with CKD deserves a plan for lab follow-up, symptom check-ins, and hydration strategy.
Practical takeaways if you’re thinking about semaglutide for kidney risk
If you’re living with type 2 diabetes, obesity, or early kidney concerns, it’s tempting to treat semaglutide like a Swiss Army knife. It’s powerful,
but it still works best as part of a bigger kidney-protection strategy.
1) Know your baseline numbers (so improvements actually mean something)
- eGFR: your trend over time is usually more important than one isolated value.
- UACR: helps detect early kidney damage and track response.
- Blood pressure: kidney outcomes and blood pressure are tightly linked.
2) Ask the “combo” question
Many people with diabetes and CKD are also on other kidney-protective therapies, such as ACE inhibitors or ARBs, and often an SGLT2 inhibitor when appropriate.
Current clinical guidance frequently emphasizes SGLT2 inhibitors as foundational for kidney protection in type 2 diabetes with CKD, with GLP-1 medicines often
added for further metabolic and cardiovascular (and increasingly kidney) benefit, depending on the individual profile.
3) Treat hydration like a real prescription
If nausea hits, don’t “tough it out” while barely sipping water. Dehydration is one of the fastest ways to turn a good long-term plan into a bad short-term
lab result. Practical strategies people often use include:
- Smaller meals and slower eating during dose escalation
- Consistent, small sips of fluids throughout the day
- Electrolyte solutions if recommended by a clinician (especially during vomiting/diarrhea)
- Promptly reporting severe GI symptoms, particularly if you have CKD
4) Keep expectations realistic (and still optimistic)
“Reduced risk” does not mean “zero risk.” CKD progression depends on many factors: genetics, blood pressure control, glucose management, smoking status,
sleep, other medications, and underlying disease processes. Semaglutide can be a meaningful tool, but it’s not a solo act.
What we still don’t know (yet)
Semaglutide’s kidney story is moving fast, but several questions remain:
- Non-diabetic CKD: SELECT suggests benefit without diabetes, but more dedicated kidney trials would strengthen confidence for broader CKD populations.
- Advanced CKD and dialysis: evidence is more limited in very low eGFR ranges and end-stage kidney disease.
- Which kidney outcomes improve most: albuminuria reduction is common; long-term kidney failure prevention is the highest-stakes endpoint and requires long follow-up.
- How benefits compare across drug classes: GLP-1 medicines and SGLT2 inhibitors both help, but they may differ in magnitude depending on baseline risk and stage of disease.
The good news is that kidney outcomes are now a front-and-center target for metabolic therapies, not an afterthought. That’s a major shift from “only glucose”
toward “whole-body risk reduction,” including the kidneys.
Bottom line
The evidence is strong that semaglutide can reduce clinically important kidney risks in adults with type 2 diabetes and chronic kidney disease,
supported by dedicated kidney outcomes data and reflected in current prescribing information for Ozempic. For Wegovy (semaglutide 2.4 mg), high-quality analyses
from major trials suggest kidney benefits in people with overweight/obesity and cardiovascular disease, even without diabetesan exciting sign that kidney protection
may extend beyond blood sugar control alone.
If you’re considering Ozempic or Wegovy with kidney health in mind, the smartest move is pairing the medication conversation with a kidney metrics conversation:
know your eGFR and UACR, manage blood pressure, ask about proven kidney-protective therapies, and take hydration seriouslyespecially during dose increases.
Your kidneys may be quiet, but they’re absolutely paying attention.
Experiences related to “Ozempic, Wegovy May Help Reduce Kidney Disease Risk” (Real-world perspective)
The clinical trial headlines are impressive, but day-to-day life is where people actually discover what semaglutide feels likeand how kidney concerns fit into the
bigger picture. Below are composite, illustrative experiences (not specific individuals) that reflect patterns clinicians commonly discuss and patients often report.
They’re meant to make the topic relatable, not replace medical advice.
Experience #1: “My labs became a storyline, not a surprise plot twist”
One common shift is that people who start semaglutide for diabetes or weight management begin paying closer attention to kidney numbers they previously ignored.
Instead of “Your eGFR is a little lowersee you next year,” appointments turn into trend-tracking: eGFR over time, UACR changes, blood pressure logs, and medication
check-ins. For many, that structure is reassuring. It feels less like waiting for bad news and more like running a long, boring marathon with a coach who actually
hands you water before you faceplant. When kidney outcomes are monitored intentionally, small improvementslike reduced albumin in the urine or slower eGFR decline
feel meaningful, because they’re tied to a plan.
Experience #2: “The nausea was real, but so was the hydration strategy”
Another frequent experience: the first weeks can be an adjustment. People often describe early nausea as “annoying but manageable,” until they realize it affects
fluid intake. Those with CKD (or borderline kidney function) may become extra aware of hydration because dehydration can make kidney labs look worse quickly.
Many end up adopting practical routines: smaller meals, more frequent sips of water, and being honest about symptoms during dose escalation. The “kidney protection”
conversation often becomes a “don’t-get-dehydrated” conversation. And while that sounds unglamorous, it can be the difference between staying on therapy comfortably
versus needing a pause due to vomiting, diarrhea, or volume depletion.
Experience #3: “Weight loss made my blood pressure meds feel… too strong”
Some people notice that as appetite decreases and weight drops, blood pressure improvessometimes enough that medications need adjusting. This is especially relevant
in CKD, where ACE inhibitors or ARBs are common and blood pressure goals can be strict. A not-unusual experience is lightheadedness when standing up, or home blood
pressure readings that suddenly look lower than expected. This isn’t a “bad side effect” so much as a “your body is changingupdate the settings” moment.
With clinician guidance, medication timing or doses may be tweaked. It’s a reminder that kidney-friendly changes often come in a bundle: weight, pressure, glucose,
and cardiovascular risk are all connected.
Experience #4: “I expected a miracle. I got momentum (and that’s actually better).”
Many people start these medications hoping for a single dramatic transformation. But a more realistic experience is gradual momentum: better fasting glucose,
less post-meal spikes, fewer cravings, improved energy, andover monthsmore stable kidney-related markers. For someone with diabetes and early CKD, hearing
“your urine albumin is down” or “your eGFR decline slowed” can feel like a win that’s hard to see in the mirror but huge on the long game. It also reframes
kidney care from fear-based (“am I headed for dialysis?”) to action-based (“what can I do this month to lower my risk?”). The therapy becomes one part of a
larger routine: nutrition, movement, blood pressure control, lab follow-ups, and sometimes additional kidney-protective medications.
Experience #5: “The best results came from teamwork, not from one pen”
A final pattern: people who do best often treat semaglutide as a catalyst, not the entire strategy. They pair it with guideline-based care: routine UACR testing,
consistent blood pressure monitoring, attention to sodium intake, and conversations about complementary therapies when appropriate. They also learn what symptoms
are worth calling aboutespecially ongoing vomiting, diarrhea, or signs of dehydrationbecause short-term kidney stress can undercut long-term gains.
In that sense, the “kidney risk reduction” story is less about a single drug and more about a new mindset: using modern metabolic tools to protect organs earlier,
before CKD becomes the loud coworker who finally demands everyone’s attention.