Table of Contents >> Show >> Hide
- Podcast-style rundown: what we’re really talking about
- Allergy immunotherapy 101 (because context is everything)
- What is intralymphatic immunotherapy (ILIT)?
- Why ILIT is getting attention now
- What the research says (and what it doesn’t)
- ILIT vs allergy shots vs SLIT: a practical comparison
- The future of allergy care: where ILIT might fit
- What to ask your allergist (the “smart patient” checklist)
- Bottom line: ILIT is promising, but it’s not magic (and that’s okay)
- Experiences from the real world (and why they matter) 500-word add-on
- SEO tags (JSON)
Seasonal allergies have a talent for showing up uninvited, redecorating your sinuses, and then charging you rent.
If you’ve ever stared at a pollen forecast like it’s a horror movie trailer, you already understand the stakes:
allergies aren’t “just sniffles” for millions of peoplethey’re missed school days, foggy work weeks, asthma flares,
and a daily pharmacy punch card.
In a KevinMD podcast episode featuring allergist-immunologist Dr. Kara Wada, the conversation turns to a topic that
sounds futuristic (and slightly like a spy gadget): intralymphatic immunotherapy, or ILIT.
The big idea is simple to say and tricky to perfect: instead of delivering allergy immunotherapy under the skin over
years, what if we could deliver tiny doses directly into a lymph nodewhere immune cells gatherusing ultrasound guidance?
This article breaks down what ILIT is, why it’s getting attention, how it compares with today’s standard allergy care,
what the research is actually showing, and what has to happen before it can become the “new normal” in the U.S.
(Spoiler: we’re not replacing allergy shots tomorrow morningbut the future is getting interesting.)
Podcast-style rundown: what we’re really talking about
Think of this as “show notes,” minus the awkward moment when someone says “Let’s unpack that” and then… doesn’t.
Here’s the core arc of the ILIT conversation:
- The problem: Allergy symptoms are common, chronic, and often under-controlled with meds alone.
- The current fix: Allergen immunotherapy worksbut it can require years of visits and persistence.
- The proposed upgrade: ILIT aims to shorten treatment dramatically by targeting the lymph node.
- The reality check: Promising trials exist, but standardization, safety technique, and U.S. adoption barriers remain.
If allergy care has a “next chapter,” it likely includes not just new medications, but new delivery strategies
that make immune training faster, safer, and easier to finish.
Allergy immunotherapy 101 (because context is everything)
What immunotherapy is trying to do
Most allergy medications are bouncers: they kick out symptoms after they’ve already crashed the party.
Allergen immunotherapy is more like training: you expose the immune system to controlled amounts of an allergen over time,
so it becomes less likely to overreact. The goal isn’t a one-day “cure,” but a longer-term reduction in symptoms and medication needs.
The main approaches used today
-
SCIT (allergy shots): In-office injections over a build-up phase followed by maintenance for years.
It’s effective, widely used, and also a time commitment that has ended many a New Year’s resolution. -
SLIT tablets: Under-the-tongue tablets for specific allergens (in the U.S., certain grass pollens, ragweed, and dust mite),
typically taken over multiple years. - SLIT drops: Used in some practices, but not FDA-approved in the U.S. for allergy treatment; coverage and standardization vary.
Here’s the bottleneck: even when immunotherapy is a great fit medically, it has to be a fit practically.
If a treatment is “effective but impossible to finish,” the real-world outcome is… people don’t finish.
That’s exactly where ILIT tries to change the game.
What is intralymphatic immunotherapy (ILIT)?
The “lymph node shortcut” in plain English
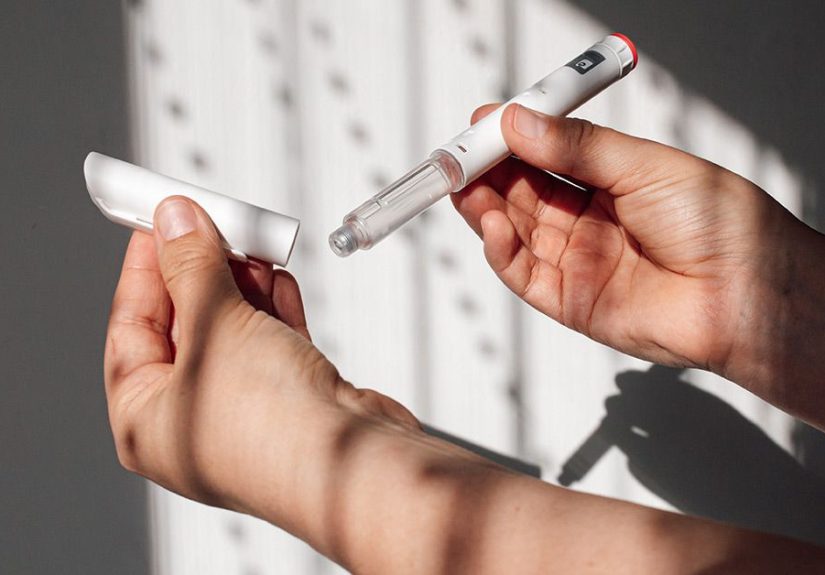
ILIT delivers allergen extract into a lymph nodeoften a superficial inguinal (groin-area) lymph nodeusing ultrasound guidance.
Lymph nodes are busy meeting rooms for immune cells. The theory is that if the allergen arrives at the meeting room,
you can use a much smaller dose and still get a strong immune-training effect.
The protocol people talk about most
A commonly discussed ILIT approach uses a three-injection protocol over a short period (often around two months),
rather than years of ongoing dosing. This is one reason ILIT is described as a potential “efficiency upgrade.”
Why ultrasound matters (and why ILIT isn’t “just another shot”)
ILIT is procedural. It requires imaging guidance to place the injection in the right spot. That makes it different from traditional allergy shots:
it’s not simply an injection scheduleit’s a technique-dependent medical procedure.
And technique matters for more than comfort: lymph nodes sit near important blood vessels, and the lymphatic system has real consequences
if injured. ILIT’s promise comes with a serious “do this correctly” warning label.
Why ILIT is getting attention now
1) Time is the hidden side effect of allergy care
Traditional allergy shots can run for 3–5 years. Even motivated patients can struggle with the logistics:
transportation, school/work schedules, and the simple reality that life happens.
ILIT’s headline appeal is straightforward: shorter treatment duration may mean more people can actually complete it.
Completion matters because immune training is a long gameif you quit early, you often don’t get the full payoff.
2) A smaller dose with a bigger immune “signal” (in theory)
Reviews of allergen immunotherapy research describe ILIT as leveraging the immune density of lymph nodes to generate immune changes
with lower doses. If that holds consistently, it could mean fewer visits and potentially fewer systemic reactionsthough safety always depends
on the allergen, the patient, and the protocol.
3) It fits the broader trend: targeted delivery
Medicine keeps moving from “more medication” to “smarter delivery.” In allergy care, that includes exploring new routes of immunotherapy
(oral mucosal approaches, intranasal approaches, patches) and combining immune training with modern biologic therapies when appropriate.
ILIT sits right in that innovation lane.
What the research says (and what it doesn’t)
Evidence highlights: encouraging signals in allergic rhinitis
ILIT has been studied most often in allergic rhinoconjunctivitis (classic seasonal “hay fever” symptoms affecting the nose and eyes).
In at least one placebo-controlled trial summarized for a public audience, a three-injection ILIT approach for grass pollen allergy
was associated with a meaningful reduction in symptoms and medication use over follow-up, with a strong effect in the first pollen season after treatment.
Safety signals: “good in trials” doesn’t automatically mean “ready for everyone”
Some trial reports describe favorable safety profiles with mostly local reactions. That’s a big dealbecause systemic reactions are a key concern
for any form of allergen immunotherapy.
But ILIT has its own unique safety considerations: it’s delivered into lymph nodes near critical anatomy.
Publications emphasizing ultrasound-guided technique warn that injuring certain superficial inguinal nodes could theoretically contribute to
lymphatic complications such as lymphedemaan uncommon but serious outcome in other medical contexts when lymphatic pathways are disrupted.
Standardization is the missing bridge
A recurring theme in immunotherapy innovation is that “promising” is not the same as “plug-and-play.” For ILIT, open questions include:
- Which allergens and extracts work best for ILIT, and at what dose?
- Which lymph node location is optimal for safety and effect?
- How should clinicians train, credential, and standardize the ultrasound-guided technique?
- What outcomes matter most: symptom scores, medication use, quality of life, or longer-term disease modification?
So… is ILIT “approved” in the U.S.?
ILIT is discussed by major allergy organizations as a newer approach and is often described as using extracts that are FDA-approved for allergy shots
but used off-label when applied in different routes. Reviews also note that ILIT is not yet an authorized routine, standardized allergy treatment
across the U.S. the way traditional allergy shots are. Translation: it’s still emerging, still evolving, and still building its evidence base.
ILIT vs allergy shots vs SLIT: a practical comparison
Convenience
- Allergy shots (SCIT): Frequent visits early, then maintenance visits; long duration.
- SLIT tablets: At-home dosing, but daily adherence for years.
- ILIT: Potentially far fewer sessionsbut each session is procedure-based and ultrasound-guided.
Access and infrastructure
Allergy shots are widely available because they rely on standardized clinic workflows. SLIT tablets are also straightforward logistically
once prescribed. ILIT requires ultrasound equipment, procedural training, and a clinic setup comfortable with image-guided injections.
That difference alone affects scalability.
Safety profile considerations
Any allergen immunotherapy can cause reactions, and patients with uncontrolled asthma or other risk factors must be carefully evaluated.
ILIT’s safety discussion adds a layer: the procedure must avoid nearby vascular structures and respect lymphatic anatomy.
Who might benefit (conceptually)
ILIT’s “best fit” populationif evidence and protocols continue to maturemay include patients who:
- Have significant allergic rhinitis/rhinoconjunctivitis symptoms despite standard medication strategies
- Are appropriate candidates for immunotherapy but struggle with multi-year schedules
- Need shared decision-making that weighs procedure logistics vs long-term time burden
This is not a self-diagnosis situation. Immunotherapy decisions should be made with a board-certified allergist
who can evaluate triggers, asthma status, reaction risk, and realistic adherence.
The future of allergy care: where ILIT might fit
1) Precision immunotherapy (less “one-size-fits-all”)
Allergy treatment is slowly moving toward personalization: matching route and regimen to the patient’s allergen profile,
symptom pattern, comorbid asthma, lifestyle constraints, and risk tolerance. ILIT adds another potential tool in that toolbox,
especially for people who need a shorter course.
2) Better formulations: peptides, adjuvants, and standardized extracts
One research direction is improving what gets deliveredpurified peptides or modified allergen components designed to reduce allergic side effects
while still training immune tolerance. If ILIT becomes more standardized, it likely won’t look exactly like today’s extract-based approaches.
3) Hybrid strategies: immunotherapy plus biologics
Modern allergy and asthma care already includes biologic medications for certain severe conditions. In the future, some patients may use biologics
to stabilize disease while immunotherapy (potentially including ILIT) retrains the immune system for longer-term benefit.
The goal would be fewer flares now, and less disease later.
4) Outcomes that matter: quality of life, not just symptom scores
The next era of allergy research is increasingly focused on real-world outcomes: sleep, school performance, sports participation,
reduced medication load, and fewer exacerbations. A therapy that is “slightly less effective” but dramatically easier to complete
could outperform a perfect therapy that most people never finish.
What to ask your allergist (the “smart patient” checklist)
If ILIT comes up in a podcast, a news story, or a clinic conversation, here are grounded questions that keep you out of hype-land:
- Is ILIT available here, and if so, what protocol and allergen extracts are used?
- What evidence exists for my specific allergen trigger (grass, ragweed, dust mite, etc.)?
- How is safety handled (observation, emergency preparedness, asthma screening, technique training)?
- How does this compare to allergy shots or FDA-approved SLIT tablets for my situation?
- What does follow-up look like after ILITbooster plans, symptom tracking, and long-term expectations?
Most importantly: don’t try to “DIY” immunotherapy decisions. Allergies can be miserable, but poorly supervised exposure
can be dangerous. Shared decision-making with a specialist is the safest path.
Bottom line: ILIT is promising, but it’s not magic (and that’s okay)
ILIT is one of the more intriguing ideas in allergy care because it attacks a real problem: treatment burden.
A shorter immunotherapy course could help more people finish immune training and get lasting relief.
Early and mid-stage studies suggest ILIT can reduce symptoms for certain aeroallergens, and technique-focused publications emphasize how to deliver it safely.
But innovation doesn’t become standard care until the details are boringly consistent: standardized protocols, larger trials,
clear patient selection, clinician training pathways, safety tracking, and outcomes that hold up in real-world settings.
For now, ILIT belongs in the “watch this space” categoryespecially if you’re the kind of person who likes their future
to include fewer tissues, fewer meds, and fewer springtime grudges against trees.
Experiences from the real world (and why they matter) 500-word add-on
When people talk about “the future of allergy care,” it can sound like a tech keynote: sleek, shiny, and suspiciously free of sneezing.
But the most useful insights usually come from lived experiencewhat patients and clinicians notice over months and years.
While individual stories vary (and your allergist is the best guide for your specific case), several patterns show up again and again
in how people experience immunotherapy, and they’re exactly why ILIT is generating buzz.
Experience #1: The time-commitment tug-of-war. Many patients start allergy shots with genuine optimism.
The first weeks feel manageable: “I can do this.” Then real life shows upexams, travel, job schedule changes, childcare, transportation,
or the simple burnout of one more appointment. Clinicians frequently see the same emotional arc: motivation → busy season → missed visits →
“I’ll restart later” → later never comes. The science of immunotherapy may be strong, but the behavioral reality is often the limiter.
That’s why the ILIT concept lands so powerfully: fewer visits could mean fewer opportunities for life to derail the plan.
Experience #2: The ‘I didn’t realize how bad it was until it improved’ effect. People living with chronic allergic rhinitis
often normalize poor sleep, constant mouth-breathing, and low-grade fatigue. After effective treatmentwhether optimized medications, shots,
or tablet therapysome describe a surprising shift: better sleep, fewer headaches, more focus, and less “always-on” congestion.
That’s a reminder that allergy care isn’t just comfort; it can ripple into school performance, mood, and everyday energy.
Any approach that improves completion rates could translate into more of these quality-of-life wins at the population level.
Experience #3: Anxiety around reactionsand reassurance from good coaching. Even though severe reactions to immunotherapy
are uncommon, the fear can be real, especially for families who have experienced asthma flares or scary allergic episodes.
Patients often feel calmer when the plan is clear: why observation periods exist, how asthma control is checked, what symptoms matter,
and what to do if something feels off. If ILIT expands, the same “good coaching” will be essentialbecause the delivery method feels more technical.
Ultrasound-guided procedures can inspire confidence (“They can see what they’re doing!”) but also nervousness (“Wait, a lymph node?”).
Clear communication will matter as much as the needle.
Experience #4: People want options that fit their life, not just their lab tests. Some patients prefer a daily tablet at home.
Others prefer periodic clinic visits because it keeps them accountable. Some have one dominant trigger (like dust mite) and a clear pathway,
while others have multiple sensitivities and need a more customized strategy. The future of allergy care likely isn’t a single “best” method
it’s a menu of evidence-based options. ILIT’s best contribution may be expanding that menu for the many people who need immunotherapy benefits
but can’t realistically commit to a multi-year schedule.
The most exciting part of ILIT isn’t that it’s flashy. It’s that it respects a truth every patient already knows:
the best treatment is the one that works and actually fits into a human life.