Table of Contents >> Show >> Hide
- What Is Athazagoraphobia?
- Symptoms of Athazagoraphobia
- Common Triggers
- Causes and Risk Factors
- How Athazagoraphobia Is Diagnosed
- Treatment for Athazagoraphobia
- Practical Coping Skills You Can Start Using
- How to Support Someone With Athazagoraphobia
- When to Seek Professional Help
- Quick FAQs
- Real-Life Experiences Related to Athazagoraphobia (and What They Teach Us)
- Conclusion
Ever had that “everyone forgot I exist” feeling after you posted something brilliant and got… two likes (one from your aunt, one from a bot)?
Now imagine that worry cranked up to maximum volume, playing on repeat, and steering your choices like an anxious GPS that keeps yelling,
“RECALCULATING… YOU’RE BEING REPLACED!”
That’s the emotional neighborhood where athazagoraphobia lives: a persistent, intense fear of being forgotten, ignored, or replaced
(and in some cases, a fear of forgetting others or losing important memories). This article breaks down what it can look like in real life,
why it may develop, how clinicians typically evaluate it, and what treatments actually help.
What Is Athazagoraphobia?
Athazagoraphobia is commonly described as an intense fear of being forgotten, overlooked, or erased from other people’s minds.
Some people also use the term for a fear of forgetting someone meaningful, or losing memories that feel like part of their identity.
Important nuance: athazagoraphobia is not a formal diagnosis label in the DSM-5-TR. That doesn’t mean the distress isn’t real.
It usually means a clinician will evaluate your symptoms and then determine which recognized condition best fitsoften something in the anxiety
family (for example, specific phobia traits, social anxiety patterns, panic symptoms, OCD-like reassurance cycles,
or anxiety tied to attachment, trauma, grief, or depression).
Think of athazagoraphobia less like a “rare, mysterious creature” and more like a descriptive headline for a fear pattern:
“My brain is convinced that being forgotten equals danger.”
Symptoms of Athazagoraphobia
Symptoms can vary from mild (nagging worry) to severe (panic, avoidance, relationship strain). Most people experience a mix of emotional,
physical, and behavioral signsespecially when a trigger shows up (a delayed text, a missed invitation, a friend getting close to someone else,
or a situation where you feel invisible).
Emotional and cognitive symptoms
- Persistent fear of being forgotten, ignored, replaced, or “left behind.”
- Ruminating on small signs (“They used a period. It’s over.”).
- Catastrophic thinking (“If they forget me, it means I don’t matter.”).
- Hypervigilance to social cues: tone changes, response times, group dynamics.
- Jealousy or panic when someone’s attention shifts elsewhere.
- Memory-focused anxiety (for some): fear of forgetting loved ones, important moments, or personal history.
Physical symptoms (the “alarm system” response)
When anxiety spikes, the body can respond like there’s an emergencybecause your nervous system doesn’t care that the “threat” is a read receipt.
Physical symptoms may include:
- Racing heart, sweating, trembling or shaking
- Shortness of breath, chest tightness
- Nausea or stomach distress
- Dizziness, tingling, chills or hot flashes
- Feeling detached, unreal, or “not present” during intense fear
Behavioral symptoms (what you do to feel safer)
- Reassurance seeking: repeatedly asking if someone cares, checking if you’re “still okay.”
- Compulsive checking: refreshing messages, monitoring views/likes, rereading chats for “evidence.”
- People-pleasing or overperforming to stay memorable (over-gifting, over-texting, overcommitting).
- Avoidance: pulling away first to avoid being “left,” skipping events where you might feel invisible.
- Clinginess or controlling behaviors in relationships (not out of maliceout of fear).
- Self-silencing: not expressing needs because “that’ll make them leave.”
Over time, these behaviors can accidentally strengthen the fear. Avoidance teaches the brain, “Yep, that was dangerous,” and compulsive checking
turns into a short-term relief loop that keeps the anxiety coming back for another round.
Common Triggers
Athazagoraphobia often flares in moments that feel like social erasure or emotional distance. Common triggers include:
- Delayed replies, being left on read, or sudden changes in communication patterns
- Friends/partners becoming closer to someone else
- Being excluded from plans, group chats, or shared rituals
- Anniversaries, birthdays, or “memory moments” not being acknowledged
- Major transitions: moving, graduation, job changes, breakups, becoming a parent
- Caring for someone with memory loss, or worries about your own memory
Causes and Risk Factors
There’s no single cause. Athazagoraphobia-like fears typically develop from a blend of temperament, learning, and life experiences.
Here are common contributors clinicians consider:
1) Attachment wounds and early experiences
If early relationships felt inconsistentlove that appeared and disappeared, caregivers who were emotionally unavailable, or environments where
attention had to be “earned”the brain may learn that connection is fragile. Later, that can look like: “If I’m not constantly present,
I’ll be erased.”
2) Loss, grief, abandonment, or sudden separation
A breakup, a death, a close friendship ending, a parent leaving, moving schoolsany major loss can plant a “forgetting equals danger” association,
especially if it happened abruptly or without closure.
3) Social rejection, bullying, humiliation, or chronic invalidation
Repeated experiences of being overlooked (“You don’t matter here”) can shape self-worth and create a hair-trigger threat response to subtle social cues.
4) Anxiety sensitivity and a “high-alert” nervous system
Some people are biologically more prone to anxiety. If your body reacts strongly to uncertainty, the fear of fading from someone’s mind can become a
powerful trigger.
5) Social media and comparison culture (yes, it counts)
Social platforms can turn attention into a scoreboard. If your anxiety already leans toward “I’m forgettable,” metrics (views, likes, streaks)
can act like gasoline on a smoldering worry.
6) Memory-related fears
For some, the fear is less about being forgotten and more about forgettingespecially after witnessing dementia in a loved one,
experiencing brain fog, or enduring high stress that makes memory feel unreliable.
How Athazagoraphobia Is Diagnosed
Because athazagoraphobia isn’t a standalone DSM label, diagnosis usually focuses on the pattern of anxiety and how it affects your life.
A clinician (psychologist, psychiatrist, or other licensed professional) typically explores:
- What you fear (being forgotten, ignored, replaced, or forgetting someone)
- How intense it is and how often it happens
- What triggers it and what you do to cope
- Functional impact: relationships, work, school, sleep, health, time spent checking or seeking reassurance
- Duration and persistence (many anxiety-related diagnoses use a “months, not days” framework)
The clinician may evaluate whether your symptoms best fit a recognized diagnosis such as:
specific phobia-style fear and avoidance, social anxiety disorder, panic disorder,
OCD-related patterns (especially reassurance/compulsive checking), separation anxiety, PTSD,
or an anxiety presentation connected to depression or trauma.
They may also recommend a medical check-in if symptoms could be amplified by physical factors (for example: thyroid issues, stimulant use,
sleep deprivation, certain medications, or substance effects). This is not to dismiss the anxietyit’s to make sure nothing is piling on.
Treatment for Athazagoraphobia
The good news: fear patterns like this are highly treatable. The most effective approaches typically target:
(1) anxious thoughts, (2) avoidance and reassurance loops, and (3) your body’s stress response.
Cognitive Behavioral Therapy (CBT)
CBT helps you identify the thoughts that spike fear (“If they don’t respond, I’m being replaced”), test how accurate they are,
and build more balanced responses. It also teaches skills for tolerating uncertaintybecause the goal isn’t to become a robot who never cares,
it’s to stop your brain from treating silence like a five-alarm fire.
In practice, CBT for athazagoraphobia may include:
- Cognitive restructuring: challenging “mind-reading” and catastrophic predictions.
- Behavioral experiments: trying a new response and observing what happens (instead of assuming disaster).
- Core belief work: addressing deeper themes like “I’m forgettable” or “I’m only lovable if I’m useful.”
Exposure Therapy (including graded exposure)
Exposure therapy helps you face feared situations in a structured, gradual wayso your nervous system can learn,
“I can handle this, and the world doesn’t end.” For athazagoraphobia, exposures are often about reducing avoidance and compulsive reassurance.
Examples (done with professional guidance, especially if symptoms are severe):
- Waiting 10 minutes before checking messages, then gradually increasing the delay
- Posting online and choosing not to monitor reactions for a set period
- Allowing a friend/partner to have independent plans without “checking in” repeatedly
- Practicing “goodbye rituals” after social events so you don’t chase reassurance afterward
- Deliberately tolerating uncertainty: “I don’t know what they’re thinkingand I can still be okay.”
The point isn’t to stop valuing connection. The point is to stop treating uncertainty like a threat to your survival.
Mindfulness-based approaches and ACT
Mindfulness and Acceptance and Commitment Therapy (ACT) can be helpful when intrusive thoughts are sticky.
Instead of wrestling every thought to the ground, you learn to notice it (“Ah, there’s my ‘I’m being forgotten’ story again”),
then choose actions aligned with your values (respect, honesty, self-care) rather than fear.
Relationship-focused therapy (when the fear shows up in attachment patterns)
If the fear is deeply tied to attachment, trust, or past relational wounds, therapy that focuses on interpersonal patterns can help.
This may include building communication skills, boundaries, and a more stable sense of self in relationships.
Medication (when appropriate)
Medication isn’t “the fix,” but it can reduce symptom intensityespecially if anxiety is severe, panic is frequent, or depression is involved.
Clinicians commonly consider:
- SSRIs or SNRIs (often first-line for anxiety disorders)
- Beta-blockers for performance-like physical symptoms in specific situations (rapid heart rate, tremors)
- Short-term anti-anxiety medications in limited cases, with careful monitoring (because some have dependence risks)
A prescriber will weigh benefits, risks, and your specific symptoms and health history. If you’re considering medication, it’s worth asking:
“What is this targetingpanic, rumination, insomnia, overall anxietyand what’s the plan for follow-up?”
Practical Coping Skills You Can Start Using
Therapy is ideal, but you can also build day-to-day skills that weaken the fear loop. Consider these as training wheels for your nervous system.
1) Name the pattern (out loud, if you can)
Try: “My athazagoraphobia is flaring.” Labeling creates distance. The thought stops being a prophecy and becomes a momentary brain weather report.
2) Create a “reassurance budget”
If you ask for reassurance 20 times a day, aim for 15not zero. Gradual reduction prevents backlash. Reassurance works like junk food:
comforting in the moment, but it doesn’t build long-term resilience.
3) Calm the body first
Slow breathing, grounding, progressive muscle relaxation, and light movement can lower the physiological alarm so your thinking brain can come back online.
The goal is not to “think your way out” of a body panic responsestart with the body.
4) Strengthen “identity anchors”
Athazagoraphobia often attacks identity: “If I’m forgotten, who am I?” Build anchors that don’t depend on someone else’s attention:
hobbies, values, routines, community, skills, and meaningful goals.
5) Reduce triggers that act like gasoline
If caffeine, poor sleep, doomscrolling, or constant social comparison intensify symptoms, treat those like controllable inputs.
You’re not “weak”you’re managing an anxiety ecosystem.
How to Support Someone With Athazagoraphobia
- Validate without feeding the loop: “I can see this feels scary,” instead of repeated over-reassurance that becomes a ritual.
- Encourage professional help if the fear is impairing life.
- Be consistent with communication when possible, but keep healthy boundaries.
- Avoid shaming (“You’re so clingy”)shame makes anxiety louder, not quieter.
When to Seek Professional Help
Consider talking to a mental health professional if the fear is persistent, causes panic, harms relationships, disrupts sleep, or leads to significant
avoidance or compulsive checking.
If you’re in immediate danger or thinking about self-harm, seek urgent support right away. In the U.S., you can call or text 988
for the Suicide & Crisis Lifeline. For treatment referrals and information, SAMHSA’s National Helpline can help connect you to services.
Quick FAQs
Is athazagoraphobia “real” if it’s not in the DSM?
Yes. The distress is real. Many commonly used terms are descriptive rather than official diagnostic labels. Clinicians focus on the symptom pattern
and impact, then match it to recognized diagnoses to guide treatment.
Can athazagoraphobia happen with depression or trauma?
Absolutely. Fear of being forgotten can be intensified by depression (low self-worth), trauma (hypervigilance), grief (loss sensitivity),
or attachment-related wounds.
Does treatment require medication?
Not always. Many people improve significantly with therapy (especially CBT and exposure-based approaches). Medication can be helpful in some cases,
particularly when symptoms are severe or co-occurring conditions are present.
How long does it take to feel better?
It varies. Many people notice meaningful progress over weeks to months with consistent treatment and practice. The core skill is learning to tolerate
uncertainty and reduce avoidance and reassurance cycles.
Real-Life Experiences Related to Athazagoraphobia (and What They Teach Us)
The word “experience” can mean a lot of things here: what it feels like in your body, how it changes your choices, and the very human ways people try
to cope. The examples below are composite-style scenariosthe kind clinicians hear all the timemeant to help you recognize patterns
and see practical paths forward.
Experience #1: “The quiet phone” panic
You send a text. Minutes pass. Then an hour. Your mind begins writing a full-length novel: They’re annoyed. They’ve moved on. I’m irrelevant.
Your body responds as if you’re in dangerracing heart, restless energy, maybe a knot in your stomach. You check the chat again. And again.
When a reply finally comes, you feel instant relief… followed by a creeping need to keep the relief coming.
What it teaches: The core issue isn’t the delayed replyit’s the meaning your brain assigns to uncertainty.
A helpful practice is “delay and decode”: delay checking by a small, planned amount, then decode the thought (“I’m being forgotten”) into a more neutral
alternative (“They might be busy; I don’t have enough data”). Over time, you build tolerance to the gap.
Experience #2: Over-performing to stay memorable
Some people cope by becoming unforgettable on purpose: always available, always helpful, always funny, always the one who organizes the plans,
always sending gifts, always saying yes. It can look successfuluntil exhaustion hits and resentment quietly moves in.
Then the fear pops up again: If I stop being useful, will I disappear?
What it teaches: Being loved for your performance is a shaky foundation. A powerful therapeutic goal is building “earned safety”
through boundaries: saying no sometimes, allowing others to initiate, and learning that your worth does not require constant output.
Experience #3: Relationship “proof hunting”
Athazagoraphobia can turn relationships into a courtroom where you’re both the defendant and the prosecutor.
You search for evidence: how fast they reply, whether they used an emoji, whether they sounded warm, whether they posted without messaging you first.
The relationship starts to feel less like connection and more like surveillancewith you trapped in the job of monitoring your own importance.
What it teaches: “Proof hunting” reduces anxiety short-term but increases it long-term. A healthier approach is values-based communication:
instead of collecting evidence, you name a need directly (“When we go quiet for days, I get anxiouscan we plan a check-in?”) and work on tolerating the
discomfort between check-ins without compulsive monitoring.
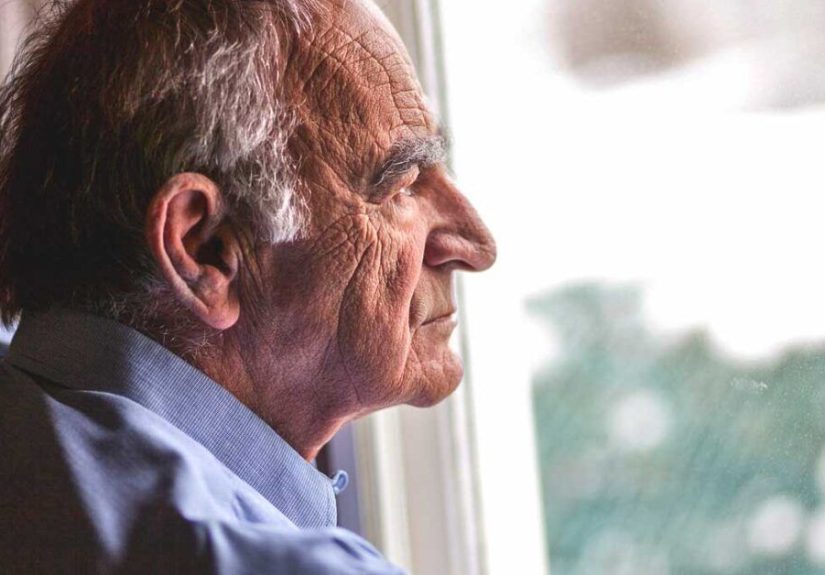
Experience #4: Caregiving and memory fear
If you’ve cared for a loved one with dementia or memory loss, the fear can become two-sided: “What if they forget me?” and “What if I forget them?”
Moments that should be tender can become charged with anticipatory grief, and your mind may obsess over preserving memoryphotos, recordings,
repeated retellinganything to keep loss at bay.
What it teaches: Memory fear is often grief in disguise. Support groups, therapy, and grief-informed coping strategies can help you hold
love and loss in the same hand. You can honor memories without turning preservation into a panic ritual.
Experience #5: The workplace invisibility spiral
At work, athazagoraphobia can show up as fear of being overlooked for projects, promotions, or recognition.
You might overwork, over-explain, or over-communicate to avoid disappearing. Or you might withdraw because visibility feels riskyif you show up and
still get ignored, it “proves” the fear.
What it teaches: The skill here is separating performance feedback from identity. Asking for clear expectations,
documenting wins, and practicing self-validation can reduce the urge to chase constant external confirmation.
Across these experiences, the theme is consistent: athazagoraphobia thrives on uncertainty plus a painful belief (“If I’m forgotten, I’m unworthy”).
Treatment helps you update that belief, retrain your nervous system, and build relationships (including your relationship with yourself) that are based
on steady values rather than constant proof.
Conclusion
Athazagoraphobia can feel deeply personallike your brain is warning you that being forgotten is the same as being unsafe.
But fear is not destiny. With evidence-based therapy (especially CBT and exposure approaches), healthy coping tools, and support that respects both
your feelings and your boundaries, it’s possible to quiet the alarm and reclaim your life from the “What if they forget me?” loop.