Table of Contents >> Show >> Hide
- Is It Really “Food Stuck,” or a Lump Feeling?
- How GERD Can Create a “Stuck” Feeling
- Other Causes That Can Look Like GERD (or Tag-Team With It)
- When “Food Stuck” Is an Emergency
- How Clinicians Figure Out What’s Going On
- Treatment: Fix the Reflux, Address the Narrowing, Calm the Throat
- A Practical “Reflux + Swallowing” Plan You Can Try
- Preventing Recurrence: Think “Maintenance,” Not “Perfect”
- Experiences People Commonly Report (and What They Often Learn)
- Conclusion
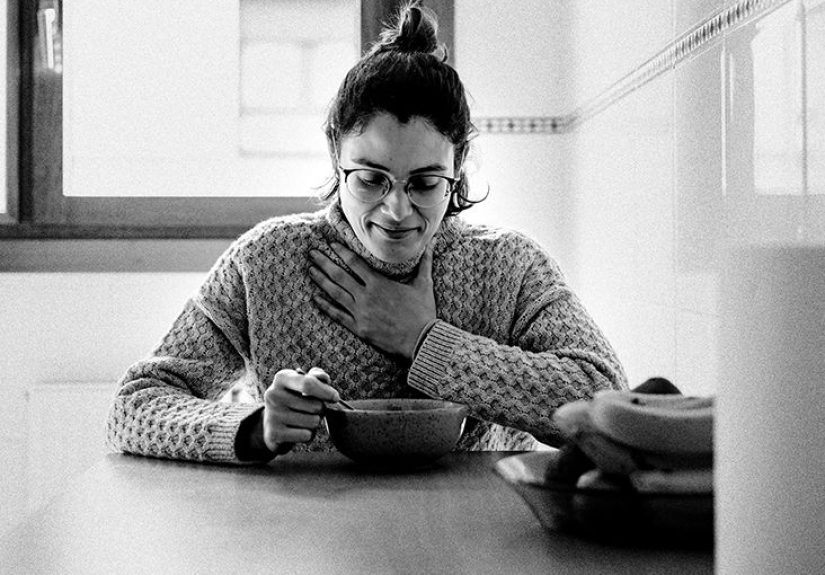
You’re enjoying a sandwich, life is good, and thenbamyour throat suddenly feels like it’s holding onto a bite like it paid rent.
If you live with GERD (gastroesophageal reflux disease), that “food stuck” sensation can be scary, annoying, and weirdly persistent.
The good news: it’s often explainable, treatable, and sometimes not actually “food stuck” at all.
In this guide, we’ll break down why GERD can make swallowing feel off, what other conditions can mimic (or team up with) reflux,
how clinicians sort it out, and the treatments that help you get back to eating without fear.
We’ll also cover the red-flag symptoms that mean you should skip the internet and get medical help right away.
Is It Really “Food Stuck,” or a Lump Feeling?
People use “food stuck in my throat” to describe a few different sensations. Separating them matters, because the causesand urgencycan be very different.
1) Globus sensation: the “lump” that isn’t food
Globus sensation feels like a lump, tightness, or something stuck in the throat even when you aren’t eating. It’s typically not painful,
and it usually doesn’t cause true difficulty moving food or liquid down. Stress, postnasal drip, throat irritation, and reflux (including
laryngopharyngeal reflux, or “silent reflux”) can all play a role.
2) True dysphagia: trouble swallowing
Dysphagia means food or liquid truly has difficulty moving from your mouth to your stomach. You might notice that solids (like meat or bread)
“hang up,” you need extra sips to get food down, or swallowing feels slower or painful. Dysphagia is considered an alarm symptom that deserves medical evaluation.
3) Food impaction: food actually stuck
Food impaction is when a solid piece of food becomes lodged in the esophagus. Some people can still swallow saliva; others can’t and may drool or spit.
This can be urgent, especially if you can’t swallow your own secretions, have chest pain, or have trouble breathing.
How GERD Can Create a “Stuck” Feeling
GERD happens when stomach contents reflux up into the esophagus. Over time, that exposure can irritate tissue, disrupt normal movement, and
sometimes cause narrowingany of which can make swallowing feel strange.
Inflammation and swelling (esophagitis)
Acid (and sometimes bile) can inflame the lining of the esophagus. Inflamed tissue can feel sensitive and “tight,” and swallowing may feel rough,
like your esophagus is protesting your dinner choices. People often describe a burning sensation, chest discomfort, or a sensation of slow passage.
Muscle spasm and hypersensitivity
Even without major visible damage, reflux can make nerves in the esophagus more sensitive. That can amplify normal sensations and trigger spasm.
Translation: the esophagus can act like a jumpy elevatorstill working, but doing it with drama.
Peptic stricture: reflux-related narrowing
Chronic reflux can lead to scarring and a narrowed segment (a peptic stricture). Strictures often cause solids to stick firstespecially dense foods
like steak, dry chicken, or crusty breadwhile liquids may still go down fine early on.
Schatzki ring (a common “stuck on steak” culprit)
A Schatzki ring is a thin ring of tissue in the lower esophagus that can narrow the opening. Many people don’t know they have it until a memorable
meal (often meat) decides to become an unexpected “core memory.” GERD and hiatal hernia can be associated with rings in some cases.
Reflux reaching the throat (LPR) and globus
Some people mainly feel reflux higher uphoarseness, throat clearing, cough, or the sensation of a lump. This can overlap with GERD and contribute to
that persistent “something stuck” feeling even when swallowing is mechanically normal.
Other Causes That Can Look Like GERD (or Tag-Team With It)
A “food stuck” sensation isn’t automatically GERD. Reflux is common, but other conditions can cause similar symptomsand some require specific treatment.
Eosinophilic esophagitis (EoE)
EoE is an inflammatory condition often linked to allergies. It can cause trouble swallowing and food impactions, and it may not improve with standard
reflux treatment alone. EoE is a big reason clinicians often take biopsies during endoscopy when dysphagia is presenteven if the esophagus looks “not that bad.”
Motility disorders (movement problems)
Your esophagus is a muscular conveyor belt. If the timing or strength of those muscle contractions is off, food can stall.
Conditions like achalasia (rare) or other motility disorders can cause both solids and liquids to feel stuck and may come with regurgitation or chest pain.
Opioid medicines can also affect esophageal motility in some people.
Esophageal cancer (less common, but important to rule out)
Most swallowing issues are not cancer, especially in younger people, but progressive dysphagia (getting steadily worse), weight loss, anemia,
vomiting blood, or black stools should be evaluated promptly.
Pill irritation and ulcers
Some medications can irritate the esophagus if they linger (for example, certain antibiotics, iron tablets, and potassium pills). Symptoms may include
pain with swallowing or a sudden onset “stuck” feeling after taking pills without enough water.
When “Food Stuck” Is an Emergency
Use common sense hereand if you’re unsure, it’s safer to get checked. Seek urgent or emergency care if you have any of the following:
- You can’t swallow saliva (drooling or needing to spit repeatedly)
- Trouble breathing, choking, wheezing, or severe coughing while trying to swallow
- Severe chest pain, especially if it’s new, intense, or comes with sweating or shortness of breath
- Vomiting blood or black/tarry stools
- Fever, severe neck/chest pain after a forceful swallow or vomiting (rare but concerning)
- Progressive worsening dysphagia or unintentional weight loss
Important safety note: if you suspect a true food impaction, don’t keep forcing bites “to push it down.”
Definitive management is often medical (sometimes endoscopic), and delaying care can increase risks.
How Clinicians Figure Out What’s Going On
The goal is to determine whether your symptoms are due to irritation (reflux), narrowing (stricture/ring), inflammation like EoE, or a motility problem.
The workup is usually stepwise.
History and symptom pattern
Clinicians often ask: Is it solids only, liquids only, or both? Is it intermittent or progressive? Is there heartburn, regurgitation, chronic cough,
hoarseness, allergies, asthma, eczema, or a history of food impactions? Those clues help narrow the possibilities.
Upper endoscopy (EGD)
Endoscopy is commonly recommended when dysphagia is present. It allows direct inspection for inflammation, rings, strictures, or masses, and it enables
biopsies to diagnose conditions like EoE. Treatment can sometimes happen during the same procedure (for example, dilation of a narrowed area).
Barium swallow (esophagram)
This imaging test can help show narrowing, rings, or certain motility patterns. It’s often used as an adjunct, and it can be especially helpful when
clinicians suspect a structural issue or need a broader functional view.
Esophageal manometry and reflux monitoring
If endoscopy doesn’t explain persistent symptoms, clinicians may use manometry (to measure muscle function) or ambulatory reflux monitoring
(to document reflux burden and correlate symptoms).
ENT evaluation (when throat symptoms dominate)
If your main complaint is a lump sensation, voice changes, or throat irritation, an ENT evaluation may be used to assess the larynx and surrounding tissues,
especially to rule out local causes.
Treatment: Fix the Reflux, Address the Narrowing, Calm the Throat
The “right” treatment depends on the cause. Many people benefit from a combination: reflux control + swallowing-friendly habits + targeted therapy when needed.
1) Lifestyle strategies that actually help
- Eat smaller meals and avoid “I skipped lunch so now I’m eating like a bear preparing for hibernation.”
- Stay upright after eating for 2–3 hours; gravity is free and surprisingly effective.
- Identify trigger foods (common ones include fatty meals, peppermint, chocolate, coffee, spicy foods, citrus, tomato-based foods, and alcohol).
- Weight management can reduce reflux pressure for some people.
- Elevate the head of the bed if nighttime symptoms are a problem (pillows alone often slump; a wedge or bed elevation can work better).
- Stop smoking if applicable; it can worsen reflux mechanisms.
2) Swallowing-friendly eating habits
These habits are especially useful if you’ve had episodes where dense foods stick:
- Slow downsmall bites, thorough chewing.
- Moisten dry foods (sauces, broth, yogurt-based dips) to reduce “dry swallow” friction.
- Alternate bites with sips if that helpsbut avoid chugging to force food down if you feel true obstruction.
- Be cautious with “high-risk bites”: steak, dry chicken, bread, rice balls, and dense sandwiches are repeat offenders.
3) Medications for GERD
Common options include antacids (quick relief), H2 blockers, and proton pump inhibitors (PPIs). PPIs are often used when symptoms are frequent, when
there’s evidence of esophagitis, or when clinicians suspect reflux is contributing to dysphagia without other alarm features.
Medication choices and timing (often before meals) matterso it’s worth discussing an individualized plan with a clinician.
4) Treating strictures and rings
If a stricture or Schatzki ring is found, endoscopic dilation may widen the narrowed area and reduce future sticking episodes. Reflux control is typically
part of long-term prevention because ongoing acid exposure can contribute to recurrence.
5) If EoE is the culprit
EoE treatment may include PPIs, swallowed topical steroids, and/or dietary approaches (often elimination diets guided by clinicians and dietitians).
The goal is to reduce inflammation and prevent remodeling (scarring/narrowing) that increases the risk of food impaction.
6) Procedures for refractory GERD (selected cases)
When symptoms persist despite optimized medical therapyor when anatomy like a significant hiatal hernia is involvedsome people consider surgical or
endoscopic anti-reflux procedures. These decisions are individualized and typically require careful evaluation and testing.
7) What to do during a mild “stuck” episode
If you feel mild sticking but can swallow normally and aren’t in distress, stop eating, stay calm, and give your esophagus time to relax.
If symptoms are severe, you can’t swallow saliva, or you’re worried about choking or chest pain, seek urgent medical care.
When in doubt, treat it like a safety issuenot a willpower contest.
A Practical “Reflux + Swallowing” Plan You Can Try
Here’s an example routine many people find helpful while they’re getting evaluated or optimizing treatment:
- Breakfast: oatmeal with banana or yogurt; avoid rushing; chew fully.
- Lunch: softer proteins (fish, shredded chicken) with cooked vegetables; avoid very dry bread or giant bites.
- Dinner: smaller portion, earlier in the evening; limit heavy/fried foods.
- Night routine: no late snacking; head-of-bed elevation if nighttime reflux hits.
- Trigger test: reduce one common trigger at a time for a week (coffee, spicy foods, etc.) to see what changes.
Preventing Recurrence: Think “Maintenance,” Not “Perfect”
GERD and throat symptoms can improve significantly, but the best results usually come from consistency:
taking medications as directed (if prescribed), keeping meals manageable, and following up if symptoms change.
If you’ve had repeated food sticking episodes, an evaluation is importanteven if heartburn is mild or absent.
Experiences People Commonly Report (and What They Often Learn)
Living with GERD plus a “food stuck” sensation tends to create a very specific emotional loop: you eat, you worry, your throat feels tighter,
and suddenly swallowing becomes something you think about all day. Many people describe the first episode as genuinely frighteningespecially when it happens
with meat or breadbecause it feels like the food has “caught” somewhere behind the breastbone. Some notice that the sensation improves after a few minutes,
while others find it lingers as soreness or irritation for a day or two.
A common experience is realizing the symptom isn’t always consistent. One day you can eat pasta with zero drama; the next day, a single bite of dry chicken
feels like it’s negotiating a cramped hallway. That inconsistency often points to intermittent narrowing (like a ring), inflammation that fluctuates,
or heightened sensitivity from reflux. People also report that speed matters: the faster they eatespecially during stressful daysthe more likely they are to
have sticking sensations. It’s not that stress “creates” a physical blockage, but tension can amplify throat and chest sensations and encourage hurried swallowing.
Many individuals also discover they were unintentionally setting themselves up for trouble with “high-risk bites”: swallowing big pieces, eating dry foods
without liquids, or talking and laughing mid-bite (a classic dinner-table betrayal). Over time, they may adopt small but effective habits:
cutting food smaller, chewing until it’s soft, and adding moisture (sauce, broth, or yogurt-based dips) to reduce friction. These changes can feel almost
too simpleuntil you realize the esophagus is not impressed by your busy schedule.
Another frequent experience is confusion between globus sensation and true dysphagia. Some people feel a constant lump even when they aren’t eating,
especially after a reflux flare, during allergy season, or when they’ve been clearing their throat a lot. They may worry that something is “stuck” 24/7,
when the underlying issue is irritation and muscle tension in the throat rather than an actual food obstruction. In those cases, reflux control, hydration,
and avoiding repetitive throat clearing can help, and reassurance after an evaluation can be surprisingly therapeutic.
People who ultimately learn they have eosinophilic esophagitis often describe a long story of “I just eat slow” or “I drink water with every bite”
that they assumed was normal. Once they start targeted treatment (such as anti-inflammatory therapy and/or dietary strategies), they’re often surprised
by how much easier eating becomesand how much anxiety around meals quietly disappears. On the flip side, people with reflux-related strictures or rings
often report dramatic improvement after dilation, followed by the realization that ongoing reflux management matters to keep symptoms from returning.
The most consistent takeaway across experiences is this: recurring food-sticking sensations deserve evaluation. Many people wish they’d gone sooner,
not because the answer was scary, but because the right diagnosis often brings reliefboth physical and mental. Eating should not feel like a risky activity,
and if it does, you deserve a plan that makes it safer and calmer.
Conclusion
GERD can absolutely contribute to a “food stuck in the throat” sensationthrough irritation, swelling, spasm, and, in some cases, narrowing like strictures or rings.
But GERD isn’t the only possible cause. Conditions like eosinophilic esophagitis and motility disorders can look similar and require targeted treatment.
If you have true dysphagia, repeated food sticking episodes, or any red-flag symptoms, get evaluated promptly. With the right diagnosis and a tailored plan,
most people can reduce symptoms dramatically and get back to eating without fear.






