Table of Contents >> Show >> Hide
- What Is Transthyretin Amyloidosis?
- Common Symptoms: How ATTR Can Show Up
- How Is Transthyretin Amyloidosis Diagnosed?
- Treatment Options for Transthyretin Amyloidosis
- Daily Life with Transthyretin Amyloidosis
- Relationships, Work, and Planning Ahead
- Real-Life Experiences: What Living with ATTR Can Feel Like
- Takeaway
Getting a diagnosis of transthyretin amyloidosis (often shortened to ATTR amyloidosis) can feel like someone just handed you a medical textbook in another language. There are new acronyms, new medications, new specialists, and a lot of questions about what daily life will look like. The good news: while ATTR is serious and progressive, treatment options and day-to-day strategies have grown quickly in the last decade, giving many people more time, better function, and a real chance to keep doing the things they love.
This guide breaks down what transthyretin amyloidosis is, how it can affect your body, the treatments you may hear about, and practical ways to manage life with the condition. Think of it as your plain-English companion to those specialist appointmentsscience-based, but also realistic about what living with ATTR actually feels like.
What Is Transthyretin Amyloidosis?
Transthyretin (TTR) is a protein made mostly in your liver. Its normal job is pretty boring (by protein standards): it helps carry thyroid hormone and vitamin A around your body. In transthyretin amyloidosis, that protein starts to misfoldessentially taking on the wrong shape. These misfolded proteins clump together into amyloid deposits that build up in organs and tissues over time.
When enough of this amyloid builds up, it interferes with how those organs work. In ATTR, the heart and the nerves are the most commonly affected, but the digestive system, kidneys, eyes, and carpal tunnel region can also be involved.
Two Main Flavors: Hereditary and Wild-Type
Doctors talk about two main types of transthyretin amyloidosis:
- Hereditary (variant) transthyretin amyloidosis (hATTR or ATTRv). This form is caused by a change (variant) in the TTR gene that you can inherit from a parent. It often involves progressive nerve damage (polyneuropathy), and many people also develop heart problems over time.
- Wild-type transthyretin amyloidosis (ATTRwt). This isn’t caused by a gene variant and tends to show up later in life, more often in men. It mainly affects the heart, leading to transthyretin amyloid cardiomyopathy (ATTR-CM).
In both types, the basic problem is the same: TTR misfolds and forms amyloid. The pattern of symptoms and best treatment approach can differ based on which organs are most affected and whether there’s a genetic variant involved.
Common Symptoms: How ATTR Can Show Up
ATTR is often called a “great imitator” because its symptoms can look like more common conditionsheart failure, carpal tunnel syndrome, diabetes-related nerve damage, or irritable bowel syndrome, for example. That’s one reason many people go years before getting a firm diagnosis.
Heart-Related Symptoms (ATTR-CM)
When amyloid deposits stiffen the heart muscle, the heart has a harder time filling and pumping. This transthyretin amyloid cardiomyopathy can cause:
- Shortness of breath with activity or when lying flat
- Swelling in the legs or abdomen
- Fatigue or reduced exercise tolerance
- Irregular heartbeat or atrial fibrillation
- Chest discomfort or feeling “full” in the chest
- Dizziness or fainting, especially on standing
Standard heart-failure medications like beta-blockers or ACE inhibitors may not be tolerated well in ATTR-CM because blood pressure can already be low. Treatment requires a tailored approach from a cardiologist familiar with cardiac amyloidosis.
Nerve and Autonomic Symptoms
In hereditary ATTR, amyloid often attacks the peripheral and autonomic nerves. That can lead to:
- Numbness, tingling, burning, or pain in the feet and hands
- Weakness or trouble with balance and walking
- Digestive changes such as diarrhea, constipation, early fullness, or nausea
- Unintentional weight loss
- Sexual dysfunction
- Blood pressure drops when standing (orthostatic hypotension), causing dizziness or near-fainting
Because autonomic nerves help control digestion, heart rate, and blood pressure, autonomic dysfunction can significantly affect quality of lifebut there are targeted ways to manage many of these symptoms.
How Is Transthyretin Amyloidosis Diagnosed?
There’s no single “one and done” test. Instead, doctors put together several pieces of information:
- Clinical exam and history. Symptoms, family history, and red flags like heart failure with thickened heart walls but low voltages on ECG raise suspicion.
- Imaging. Echocardiograms, cardiac MRI, and nuclear medicine bone scans (such as technetium pyrophosphate scans) can show a pattern typical of ATTR-CM.
- Blood and urine tests. These rule out light-chain (AL) amyloidosis, another type that requires very different treatment.
- Genetic testing. A blood test can check for variants in the TTR gene, confirming hereditary ATTR.
- Biopsy in select cases. A small sample of tissue (from fat, nerve, or heart) may be examined under a microscope to confirm amyloid and determine its type.
Early diagnosis matters. Some disease-modifying therapies work best when started before there is severe organ damage, which is why specialists emphasize recognizing ATTR earlier in the disease course.
Treatment Options for Transthyretin Amyloidosis
For years, there were no targeted treatments for ATTR. That landscape has changed dramatically. While there’s still no cure, several medicines now focus on either stabilizing TTR, reducing its production, or (in research settings) clearing deposits.
TTR Stabilizers: Helping the Protein Hold Its Shape
Tafamidis (Vyndaqel/Vyndamax) is a TTR stabilizer that helps keep transthyretin in its normal shape, reducing the tendency to misfold and form amyloid. It is FDA-approved to treat cardiomyopathy caused by ATTR in adults and has been shown to reduce hospitalization and improve survival compared with standard care alone.
Other stabilizers, such as acoramidis, are being studied in clinical trials and may expand options in the future.
RNA-Silencing Therapies: Turning Down TTR Production
Another group of drugs works “upstream,” telling the liver to make less transthyretin in the first place. These include RNA-based therapies like:
- Patisiran (Onpattro)
- Vutrisiran (Amvuttra)
- Inotersen
- Eplontersen
Patisiran, vutrisiran, inotersen, and eplontersen are FDA-approved for adults with hereditary ATTR with polyneuropathy. Clinical trials show these drugs can slow or improve nerve damage and help preserve function.
More recently, vutrisiran (Amvuttra) has also been approved for ATTR-CM, offering an additional option for people with heart involvement. It is given as a subcutaneous injection every three months.
In a major trial, patisiran preserved walking distance and quality-of-life scores over 12 months in people with ATTR cardiac involvement, highlighting the potential of these drugs to stabilize disease.
Liver Transplant and Other Approaches
Because most transthyretin is made in the liver, liver transplantation was historically used to treat hereditary ATTR. Transplanting a new liver reduces production of the abnormal TTR, though it doesn’t remove existing deposits and is now less common thanks to modern medications.
Other approaches under study include monoclonal antibodies that help clear amyloid deposits and gene-editing technologies that may one day dramatically reduce TTR production with a single treatment. These are exciting, but still largely in the research phase.
Supportive Care: The Foundation of Living Well with ATTR
Even with disease-modifying therapy, supportive care remains essential:
- Careful use of diuretics and sodium restriction to manage heart-failure symptoms and fluid retention
- Compression stockings and medications like midodrine for blood pressure drops
- Neuropathic pain medications, physical therapy, and assistive devices to maintain mobility
- Targeted treatment for digestive symptoms, including small, frequent meals and medications for diarrhea or constipation
Because ATTR is multisystem, many people benefit from a team that includes a cardiologist, neurologist, gastroenterologist, and sometimes a genetic counselor, dietitian, and physical therapist.
This article is for general information only. Your specific treatment plan should be personalized by your healthcare team based on your type of ATTR, organs involved, and other health conditions.
Daily Life with Transthyretin Amyloidosis
You can’t control the fact that you have transthyretin amyloidosisbut you do have some control over how you live with it. Small, consistent habits can make a surprisingly big difference in your energy, symptoms, and independence.
Eating for Your Heart and Nerves
There’s no special “ATTR diet,” but certain patterns help support heart and nerve health:
- Heart-healthy basics. Focus on fruits, vegetables, whole grains, beans, nuts, seeds, and lean proteins like fish and poultry. Limit processed foods, added sugars, and fried foods.
- Watch sodium (with your doctor’s guidance). If you have ATTR-CM, your care team may recommend limiting salt to help control fluid buildup and symptoms like swelling and shortness of breath.
- Prioritize enough calories and protein. Digestive symptoms and early fullness can make it easy to lose weight. Small, frequent meals and nutrient-dense snacks can help maintain strength.
- Hydration with a plan. In heart failure, more water isn’t always better. Follow your cardiologist’s guidance on daily fluid limits.
If you’re struggling with appetite, weight loss, or fluid restrictions, a registered dietitian familiar with heart disease or rare conditions can help you create a realistic plan.
Staying Physically Active Without Overdoing It
Exercise may sound impossible when you’re short of breath or dealing with neuropathy, but gentle activity actually supports heart health, muscle strength, and mood.
Consider:
- Short walks broken into several sessions instead of one long one
- Chair exercises, light resistance bands, or water-based activities
- Working with a physical therapist who understands cardiac and neurologic limitations
The goal isn’t to become an athleteit’s to keep your body as strong and flexible as possible while respecting your limits. If symptoms like chest discomfort, severe shortness of breath, or dizziness show up, stop and let your care team know.
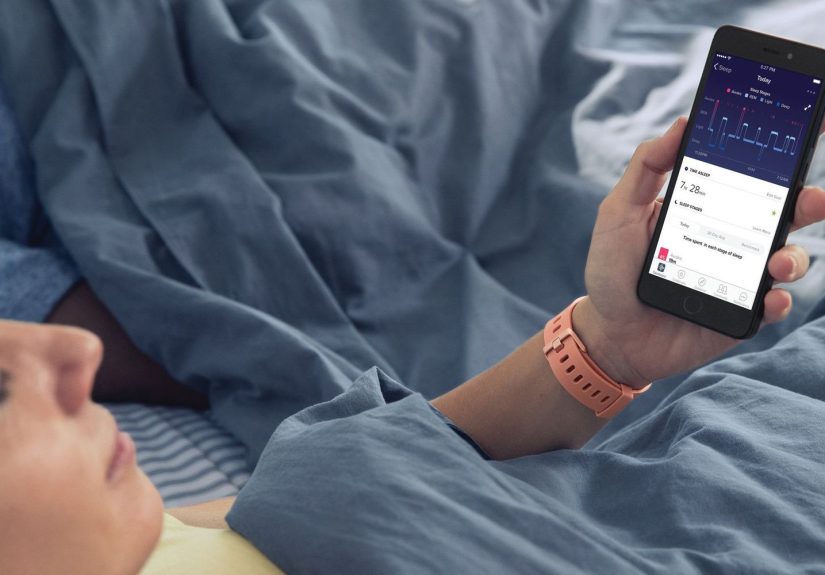
Sleep, Stress, and Mental Health
Living with a rare, chronic illness is emotionally demanding. Many people with ATTR describe feelings of uncertainty, frustration, or grief for the life they expected to have. That’s normaland it doesn’t mean you’re failing to “stay positive.”
Helpful strategies include:
- Keeping a consistent sleep routine and creating a dark, cool, quiet sleep space
- Using pillows or an adjustable bed to ease shortness of breath at night
- Relaxation practices like deep breathing, guided imagery, or gentle stretching before bed
- Talking with a therapist, counselor, or support group familiar with chronic illness
Online communities for people with amyloidosis can provide both practical tips and emotional validationyou’re not the only one navigating this.
Working with Your Healthcare Team
Because ATTR often involves multiple organs, you may collect specialists the way some people collect houseplants. To keep things manageable:
- Use one notebook or app to track symptoms, questions, and medication changes.
- Bring a list of your top 3 concerns to each appointment so they don’t get lost in the details.
- Ask who is acting as your “quarterback”often an amyloidosis specialist or cardiologist who helps coordinate care.
- Consider bringing a family member or friend to important visits as a second set of ears.
Shared decision-makingwhere you and your clinicians discuss options, preferences, and trade-offs togetheris especially important with rare diseases like transthyretin amyloidosis.
Relationships, Work, and Planning Ahead
ATTR doesn’t just affect organs; it affects schedules, roles, and plans. Communication can help you adjust together.
- With family and friends. It can be hard for others to understand an illness that’s mostly invisible. Sharing short, concrete examples (“By afternoon I hit a wall of fatigue” or “Standing in line can make me dizzy”) can help people grasp what you’re dealing with.
- At work. Some people continue working with reasonable adjustments like flexible hours, remote work days, or reduced travel. Others transition to part-time or disability. A social worker or patient-advocacy organization can help you understand options.
- Planning for the future. As treatments improve, many people with ATTR are living longer, more active lives. At the same time, it’s wise to discuss advance care planning, financial matters, and who you’d want making decisions if you couldn’t. Doing this early can reduce stress later.
Real-Life Experiences: What Living with ATTR Can Feel Like
Every person with transthyretin amyloidosis has a different story, but many experiences overlap. The following composite examples are based on common themes reported by people living with ATTR and their care teams.
“I Thought It Was Just Getting Older”
Maria, a fictional 62-year-old teacher, spent years blaming her fatigue on a busy schedule and “getting older.” When climbing stairs left her breathless and her ankles started to swell by mid-day, she was told she had heart failure. Standard medications didn’t sit wellher blood pressure dropped, and she felt even worse.
Eventually, a cardiologist noticed that her heart walls were thickened on imaging in a way that didn’t fit typical high-blood-pressure disease. A nuclear scan and blood tests led to a diagnosis of transthyretin amyloid cardiomyopathy. Starting tafamidis and carefully adjusting diuretics helped her breathe easier. She still paces herself and avoids long days on her feet, but she can teach part-time, go for short walks with her grandchildren, and plan lessons again instead of planning around her symptoms.
“Neuropathy Was the First Clue”
James, a fictional 55-year-old mechanic with a strong family history of “mysterious nerve problems,” started having burning pain in his feet and trouble buttoning shirts. At first, he was told it was likely related to prediabetes. But as his symptoms climbed up his legs and he developed digestive issues and erectile dysfunction, his neurologist dug deeper.
Genetic testing revealed a TTR variant, confirming hereditary transthyretin amyloidosis with polyneuropathy. James began a TTR-lowering therapy along with medications for nerve pain and physical therapy to improve balance. He switched from full-time mechanic work to a role ordering parts and managing the front office, which allowed him to stay in a field he loved while protecting his function.
For James, one of the biggest changes was psychological. Naming the conditionand learning about targeted treatmentsreplaced a vague fear of “something terrible we can’t fix” with a clearer roadmap. He still has to pace activities and use a cane on bad days, but he feels more in control and less alone.
Small Adjustments, Big Impact
People living with ATTR often describe a shift from asking “What can’t I do anymore?” to asking “How can I adapt this so it still works for me?”
- Planning errands earlier in the day, when energy is higher
- Using mobility aids or elevators without guiltit’s about preservation, not defeat
- Booking travel with wheelchair assistance at airports and extra time between connections
- Scheduling a “recovery day” after big events like weddings or family reunions
- Leaning on friends, family, faith communities, or support groups for emotional backup
None of these changes erase the reality of transthyretin amyloidosis. But together, they help many people maintain independence, connection, and a sense of selfwhile powerful new therapies work quietly in the background to slow the disease.
Takeaway
Living with transthyretin amyloidosis is not simple. It asks you to learn new language, juggle appointments, monitor symptoms, and make thoughtful choices about energy, food, movement, and treatment. But you’re not starting from zero: there are now multiple disease-modifying options, clearer diagnostic pathways, and growing experience among specialists in cardiac and hereditary amyloidosis.
By building a strong partnership with your healthcare team, adjusting daily habits to protect your heart and nerves, and reaching out for emotional support, you can move from feeling overwhelmed to feeling informed and engaged in your care. ATTR is part of your lifeimportant, yesbut it does not have to be the only story you’re living.