Table of Contents >> Show >> Hide
- What is lumbar decompression surgery?
- Common uses: When lumbar decompression is considered
- Who is (and isn’t) a good candidate?
- What happens during surgery (in plain English)?
- Success rate: What does “successful” really mean?
- What affects your odds of a great result?
- Risks and possible complications
- Recovery timeline: What most people can expect
- Specific examples: What success might look like
- Questions to ask your surgeon
- Real-World Experiences: What recovery often feels like (and what people wish they knew)
- The “I woke up and the leg pain was gone!” moment (sometimes)
- The “Why does my leg still feel weird?” phase (also normal)
- Walking becomes the unexpected hero
- Energy and mood: the hidden recovery variables
- Physical therapy: not punishment, more like a user manual for your new space
- What people commonly say helped
- Conclusion
If your lower back has been running a full-time “pinch-the-nerve” operationshooting pain down your leg, making your feet tingle, or turning a simple grocery run into a
sit-down-and-cry-in-aisle-7 experienceyour doctor may bring up lumbar decompression surgery.
It’s not a magic wand, but for the right person, it can be a very practical, very evidence-based way to give compressed nerves more space and restore function.
This guide breaks down what lumbar decompression surgery is used for, what “success” actually means (spoiler: it’s not always “zero pain forever”),
and the real-world factors that affect outcomeslike diagnosis, technique, fitness, and expectations.
We’ll keep it accurate, in-depth, and just funny enough that your spine won’t file a complaint.
What is lumbar decompression surgery?
Lumbar decompression surgery is a category of procedures designed to relieve pressure on spinal nerves in the lower back (lumbar spine).
When the spinal canal or nerve tunnels narrowoften from age-related changesnerves can get squeezed.
Decompression surgery creates more room by removing or trimming the structures causing that crowding.
You might hear decompression described with specific procedure names, such as:
- Laminectomy: removing part or all of the lamina (the “roof” of the spinal canal) to widen the canal.
- Laminotomy: removing only a portion of the lamina (a smaller “window” compared to laminectomy).
- Foraminotomy: widening the foramina (openings where nerve roots exit the spine).
- Discectomy / microdiscectomy: removing herniated disc material that presses on a nerve root.
- Decompression with fusion: decompression plus stabilizing the spine with hardware and bone graft when instability is present or likely.
Surgeons may perform these as open procedures or using minimally invasive techniques. The “best” approach depends on your anatomy,
symptoms, imaging, and stabilitynot on what has the coolest acronym.
Common uses: When lumbar decompression is considered
Lumbar decompression is usually recommended when symptoms are clearly linked to nerve compression and conservative care hasn’t provided enough relief.
The most common “uses” include:
1) Lumbar spinal stenosis (the classic reason)
Lumbar spinal stenosis is narrowing of the spinal canal that can compress nerves.
A hallmark symptom is neurogenic claudication: leg pain, heaviness, numbness, or weakness that worsens with standing/walking and improves with sitting or bending forward.
If this pattern sounds familiar, you’re not alonestenosis is one of the most common reasons older adults consider lumbar spine surgery.
2) Herniated disc with leg pain (sciatica) or neurologic deficits
A disc herniation can press on a nerve root and cause radiating leg pain (often called sciatica), numbness, tingling, or weakness.
Many cases improve without surgery, but decompression (often microdiscectomy) may be recommended when symptoms are severe, persistent, or associated with progressive weakness.
3) Bone spurs and arthritic changes (degenerative disease)
Arthritis can lead to bone spurs and thickened ligaments that narrow nerve pathways.
Decompression can remove or shave these structures to reduce compression.
4) Spondylolisthesis (vertebra slip) with stenosis
In degenerative spondylolisthesis, one vertebra slips slightly forward relative to another, often alongside stenosis.
Some patients do well with decompression alone; others may need decompression plus fusion, especially if there’s instability.
This is one of the most debated “it depends” areas in spine careand your imaging, symptoms, and stability matter a lot.
5) Less common uses
Lumbar decompression may also be used for certain spinal cysts, tumors, or infections that compress nervesthough these are less common and require individualized planning.
Who is (and isn’t) a good candidate?
A strong candidate typically has:
- Leg-dominant symptoms (pain, numbness, tingling, weakness) that match a specific compressed nerve pattern.
- Imaging evidence (MRI/CT) that matches symptoms (not just “wear and tear” that many people have without pain).
- Functional limitation (walking distance shrinking, daily activities becoming difficult).
- Failure of appropriate non-surgical care (activity modification, physical therapy, medications, and/or injections when appropriate).
Decompression may be a weaker fit when pain is mostly low back pain without leg symptoms, when imaging doesn’t match symptoms, or when broader issues
(severe deconditioning, uncontrolled diabetes, smoking, untreated osteoporosis, or significant untreated mental health stressors) are likely to reduce recovery quality.
That doesn’t mean “no,” but it does mean “let’s optimize the odds.”
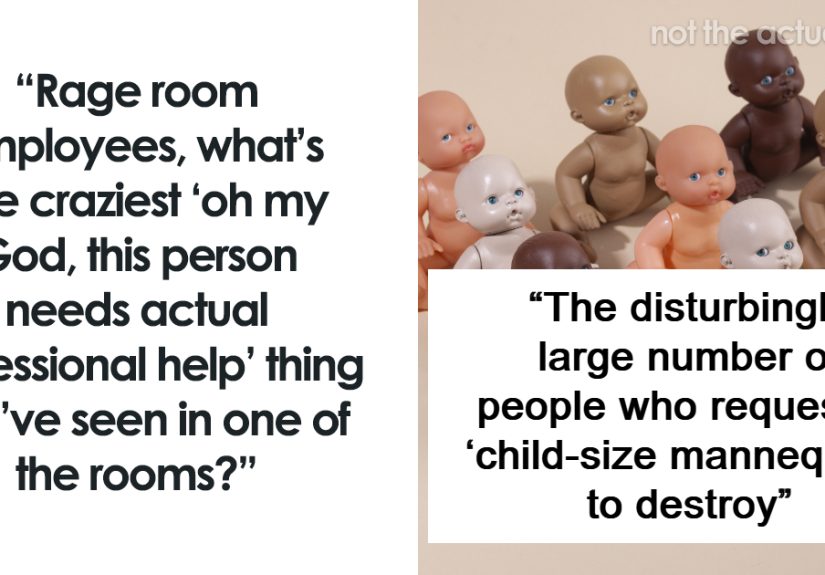
What happens during surgery (in plain English)?
The goal is simple: remove the pinch without creating instability.
Depending on the cause, the surgeon may remove part of bone, ligament, disc material, or bone spurs.
Many decompressions are done under general anesthesia. Some are outpatient; others require a short hospital stay, especially when multiple levels are treated or when fusion is involved.
A helpful mental model: think of your nerves like a garden hose. Stenosis and herniated discs are like stepping on the hose.
Decompression is moving your foot off the hoseso water (nerve signals) can flow again.
It doesn’t replace a worn-out faucet, reroute your plumbing, or promise your neighbor stops revving a motorcycle at 2 a.m. But it can fix the squeeze.
Success rate: What does “successful” really mean?
“Success” in lumbar decompression surgery usually means:
- Reduced leg pain (often the most reliable improvement).
- Improved walking tolerance and daily function.
- Better quality of life and ability to return to activities.
- Stable neurologic status (preventing worsening weakness or nerve damage when compression is severe).
It does not always mean:
- “My back will feel 17 again.”
- “I will never get sore after standing too long.”
- “I can deadlift a refrigerator next weekend.”
Typical outcomes for lumbar stenosis decompression
Across many studies and clinical summaries, a large majority of properly selected patients report meaningful improvement after decompression for lumbar spinal stenosis.
A commonly cited range is that about 70–80% of patients have significant symptom improvement, with satisfaction often landing in a similar neighborhood.
Some clinical summaries cite success rates up to around 90% for laminectomy in appropriate candidates, though “success” definitions vary.
Reoperation rates: The part nobody puts on a billboard
Some patients eventually need additional surgery, such as repeat decompression, fusion for developing instability, or treatment for adjacent-level degeneration.
Research has reported cumulative reoperation rates around the mid-teens at 5 years after surgery for lumbar stenosis in certain cohorts,
with longer-term follow-ups in some studies showing reoperation rates that can rise over time.
This doesn’t mean surgery “failed”it means spines are living structures, not one-time home renovations.
Decompression alone vs. decompression with fusion
For patients who have stenosis plus degenerative spondylolisthesis, whether to add fusion depends largely on stability and symptom patterns.
Multiple randomized studies have found that decompression alone can be non-inferior to decompression with fusion for many patients over a couple of years,
while some trials show small differences in certain outcome measures and different reoperation patterns.
Translation: there isn’t one universal answeryour case (including instability on imaging and mechanical back pain) drives the decision.
What affects your odds of a great result?
1) The diagnosis and symptom pattern
Decompression tends to shine when symptoms are nerve-driven and leg-dominant:
walking limits from stenosis, classic sciatica, and focal nerve compression patterns.
If your main complaint is generalized low back pain without clear nerve compression, decompression alone may not target the true pain generator.
2) Duration and severity of nerve compression
Nerves can recover, but very prolonged or severe compression may take longer to improveand sometimes doesn’t fully reverse.
Early evaluation is especially important if there is progressing weakness.
3) Overall health and risk factors
Smoking, poorly controlled diabetes, obesity, and low fitness can increase complication risk and slow recovery.
Improving strength, walking tolerance, and nutrition before surgery (when possible) is like upgrading your recovery “operating system.”
4) Surgical technique and the “right amount” of decompression
The goal is enough decompression to relieve symptoms while preserving stability.
Overly aggressive bone removal can increase instability; under-decompression can leave symptoms.
This is one reason experience, imaging review, and careful planning matter.
5) Expectations (the underrated success factor)
Patients who do best often have clear, functional goals:
“Walk 20 minutes,” “Stand to cook dinner,” “Sleep without leg pain,” “Get back to hiking shorter trails.”
When success is defined realistically, it’s easier to measureand celebrate.
Risks and possible complications
Any surgery has risks. With lumbar decompression, potential complications can include infection, bleeding, blood clots, nerve injury, and spinal fluid leak.
There may also be persistent symptoms, recurrent stenosis, or instability requiring further treatment.
The best way to think about risk is not “Will something go wrong?” but “How do we reduce risk?”
That includes medical optimization, careful surgical selection, and a good rehab plan.
Recovery timeline: What most people can expect
Recovery varies by procedure type (single-level vs multi-level, minimally invasive vs open, decompression alone vs fusion) and by your baseline health.
But broadly:
- First days: walking is encouraged early; soreness is expected; leg symptoms may improve quickly or gradually.
- First 2–6 weeks: steady increase in activity; restrictions on bending, lifting, twisting may apply; physical therapy may start.
- 6–12 weeks: many people build strength and endurance; walking distance often improves; lingering nerve irritation can fade slowly.
- 3–6 months: big functional gains often stabilize; some people continue improving beyond this window.
One important nuance: nerves can be dramatic. Some people feel immediate leg pain relief; others improve in steps.
A temporary “flare” of nerve symptoms during healing can happen and should be discussed with your surgeon, especially if severe or worsening.
Specific examples: What success might look like
Example A: Lumbar stenosis with neurogenic claudication
A 68-year-old who can only walk five minutes before leg heaviness and burning starts may undergo a multi-level laminectomy.
A “successful” outcome might be walking 20–30 minutes with manageable soreness, needing fewer breaks, and returning to errands and social activities.
Back stiffness may persist, but function improves dramatically.
Example B: Herniated disc with sciatica
A 42-year-old with severe radiating leg pain and numbness due to a disc herniation may have a microdiscectomy.
A strong result could be major leg pain relief within days to weeks, with gradual return to exercise and careful strengthening to reduce recurrence risk.
Example C: Stenosis plus degenerative spondylolisthesis
A 72-year-old with stenosis and a stable grade I slip might do well with decompression alone if imaging suggests stability.
Another patient with clear instability and mechanical back pain may benefit more from decompression plus fusion.
“Success” is matching the right operation to the right spine.
Questions to ask your surgeon
- What structure is compressing the nerve, and at which level(s)?
- Which procedure are you recommending (laminectomy, laminotomy, foraminotomy, discectomy) and why?
- Do you think I need fusion? What signs of instability do you see?
- What is the expected improvement: leg pain, walking distance, weakness, numbness?
- What are my complication risks based on my health factors?
- What restrictions will I have, and when can I return to work/driving/exercise?
- What is your plan if symptoms don’t improve as expected?
Real-World Experiences: What recovery often feels like (and what people wish they knew)
Let’s talk about the part that doesn’t fit neatly in a brochure: lived experience. These aren’t medical promisesjust common patterns patients report and clinicians
frequently see when lumbar decompression is done for the right reason.
The “I woke up and the leg pain was gone!” moment (sometimes)
Some people describe immediate relief of sharp, electric leg pain right after surgerylike someone finally unplugged the nerve from a wall socket.
That’s more common when the main problem was mechanical compression and the nerve wasn’t irritated for too long.
Even then, it’s normal to feel surgical soreness in the back area, becauseplot twistsurgery involves a lot of “being operated on.”
The “Why does my leg still feel weird?” phase (also normal)
Others notice that pain improves but numbness or tingling lingers. That’s not automatically a red flag.
Nerves can be slow to calm downespecially if they were compressed for months.
Many patients describe recovery as a dimmer switch, not an on/off button: one week you can walk to the mailbox, the next week you realize you can loop the block.
Walking becomes the unexpected hero
A common “aha” moment after decompression for stenosis: walking becomes possible again without the old leg heaviness.
People often start with short, frequent walkssometimes just minutes at a timeand build up gradually.
The best stories aren’t always “I ran a marathon.” They’re “I went to a museum and didn’t spend the day hunting for benches.”
Energy and mood: the hidden recovery variables
Patients often underestimate fatigue. Even if the incision is small, healing takes energy.
Some people feel great for a few days and then hit a “recovery wall” where they need naps and feel frustrated.
That’s not weaknessit’s biology. Planning for rest and support (meals, rides, help with chores) can make the experience smoother and less stressful.
Physical therapy: not punishment, more like a user manual for your new space
Many patients say they wish they had taken rehab more seriously earliernot with extreme workouts, but with consistent basics:
gentle mobility, core stability, hip strength, and posture habits.
The goal isn’t to “protect your back forever” like it’s a priceless vase; it’s to teach your body to move confidently again.
People who build strength gradually often feel more in control and less fearful of normal movement.
What people commonly say helped
- Clear goals: “Walk 15 minutes comfortably” beats “never feel anything again.”
- Small daily wins: increasing walking by a few minutes, standing a bit longer, sleeping better.
- Good questions: knowing what symptoms are expected versus what needs a call to the office.
- Patience with nerves: improvement can continue for weeks or months, especially for numbness.
- Health upgrades: better blood sugar control, smoking cessation, protein intake, and gentle conditioning.
The most consistent “success stories” are less about superhero comebacks and more about getting normal life back:
walking the dog, shopping without dread, sitting through a grandkid’s school event, or traveling without planning the entire day around pain.
If that’s your goal, you’re speaking the language decompression surgery understands.
Conclusion
Lumbar decompression surgery is most often used to treat nerve compression from lumbar spinal stenosis or herniated discs, aiming to reduce leg symptoms,
improve walking and function, and protect neurologic health when needed.
Success rates are generally strong for properly selected patientsespecially when symptoms match imaging and the primary issue is nerve compression.
The best outcomes come from the right diagnosis, the right procedure, good health optimization, and realistic, functional expectations.
If you’re considering surgery, focus on a clear match between symptoms and imaging, ask smart questions about stability and technique, and treat rehab like a partnership
not an afterthought. Your spine has carried you this far. It deserves a plan, not a gamble.