Table of Contents >> Show >> Hide
- A quick snapshot: the “headline numbers” (with plain-English context)
- What counts as obesity in the U.S.? (And why BMI is useful… and imperfect)
- Reading obesity statistics like a pro (without needing a PhD)
- Who is most affected? Patterns by age, income, education, and race/ethnicity
- Why obesity is so common in America: it’s not one thingit’s the whole pinball machine
- 1) Food environments that make “extra calories” the default setting
- 2) Ultra-processed foods: engineered for convenience (and often, overconsumption)
- 3) Stress, sleep, and the “always-on” modern brain
- 4) Health conditions and medications
- 5) Built environments: when “just go for a walk” isn’t realistic
- Health impacts: why the data matters (without scare tactics)
- Myths that won’t die (even though they really should)
- What actually helps: realistic prevention and support (no detox teas, no punishment workouts)
- Where the story may be heading: the next chapter of obesity in America
- Experiences: what obesity can feel like in everyday American life (composite snapshots)
America loves big things: big highways, big dreams, big cups of iced coffee you could swim laps in.
Unfortunately, one “big” trend we’d happily downsize is obesity. And nothis isn’t a finger-wagging lecture
with a sad salad and a whistle. It’s a fact-based, human-friendly look at what obesity in the U.S. actually
looks like right now, why it’s so common, who it affects most, and what the numbers really mean.
Important tone check: bodies are not moral report cards. Obesity is a complex, chronic health condition shaped by
biology, environment, stress, sleep, medications, culture, and the daily reality of modern life. So we can talk
about obesity facts in America without shaming anyonebecause shame has never once lowered a national statistic.
A quick snapshot: the “headline numbers” (with plain-English context)
Adult obesity is still around 2 in 5 Americans
Recent national survey data show adult obesity prevalence around 40%. One CDC/NCHS analysis reported
40.3% of U.S. adults had obesity during August 2021–August 2023. That’s roughly
two out of every five adultsif you imagine a group photo, that’s not a “small corner of the room” issue; it’s a
“half the room is deciding where to order lunch” issue.
Childhood obesity affects about 1 in 5 kids and teens
Among U.S. children and adolescents ages 2–19, obesity prevalence was 19.7% from 2017 to March 2020,
which translates to about 14.7 million young people. Childhood obesity is especially important because
it can affect health right now and increases the odds of obesity continuing into adulthood.
Where you live still matters
CDC’s adult obesity prevalence maps (based on large state-level surveys) show that obesity is common everywhere, but
not evenly distributed. In 2024, every U.S. state and territory measured had an adult obesity prevalence
of 25% or higher. The Midwest and South had the highest overall prevalence.
Two statesMississippi and West Virginiawere at 40% or higher in 2024.
Severe obesity is rising (even when overall obesity looks “stable”)
“Severe obesity” typically refers to a BMI at or above 40 for adults. CDC/NCHS reported severe obesity prevalence of
9.4% during August 2021–August 2023. Even more telling: over the last decade in that analysis,
overall adult obesity didn’t change significantly, but severe obesity increased. Translation: the average headline number can
look steady while the more medically risky end of the spectrum grows.
What counts as obesity in the U.S.? (And why BMI is useful… and imperfect)
The definition most stats use
In most U.S. public health reporting, adult obesity is defined as body mass index (BMI) of 30 or higher.
Overweight is typically BMI 25 to 29.9. Severe obesity is often BMI 40 or higher.
BMI is a screening tool, not a full biography
BMI is popular because it’s easy: height and weight in, category out. But it doesn’t directly measure body fat,
doesn’t account for differences in muscle mass, and can misclassify some people. That’s why good health care looks at
more than one numberblood pressure, blood sugar, cholesterol, sleep, fitness, stress, family history, and more.
Reading obesity statistics like a pro (without needing a PhD)
Measured vs. self-reported data
Some national surveys (like NHANES) measure height and weight in person. Others (like BRFSS state maps) rely on
self-reported height and weight. Self-reported numbers can underestimate weight and overestimate height a bithuman nature plus tape-measure optimism.
That’s why adult obesity statistics can vary depending on the source, timeframe, and method.
“Prevalence” is not “new cases”
Prevalence is the share of people who have obesity at a given time. It tells you how widespread the condition is,
not how many people developed it last week. Think of it like a wide-angle photo, not a time-lapse video.
Who is most affected? Patterns by age, income, education, and race/ethnicity
Adults: middle age is a hotspot
CDC/NCHS data show adult obesity is highest among adults ages 40–59. In the August 2021–August 2023 period,
obesity prevalence for ages 40–59 was reported at 46.4%, higher than younger adults and older adults.
Busy-career years, family responsibilities, stress, sleep deficits, and less time for movement can be a perfect storm.
Education and income: the gradient is real
Obesity is more common where resources are tighter. CDC/NCHS reported lower obesity prevalence among adults with a bachelor’s degree or higher
compared with less education. For children, CDC data show obesity prevalence rises as family income decreasesan important reminder
that obesity is not simply an “individual choices” story; it’s also an “access, time, and affordability” story.
Childhood differences by age and race/ethnicity
CDC’s childhood obesity facts show obesity prevalence increased with age (highest among adolescents). The same CDC summary reports higher prevalence
among Hispanic children and non-Hispanic Black children compared with non-Hispanic White and non-Hispanic Asian children.
These differences are shaped by layered factors: food environments, marketing exposure, stress, sleep, neighborhood safety for outdoor play,
household schedules, and access to preventive care.
Why obesity is so common in America: it’s not one thingit’s the whole pinball machine
1) Food environments that make “extra calories” the default setting
Many neighborhoods make the easiest option the most calorie-dense option: convenience stores, fast-food density, large portions,
and heavy marketing. Add long work hours and commuting, and “cook a balanced dinner” can become “eat something with a steering wheel logo.”
2) Ultra-processed foods: engineered for convenience (and often, overconsumption)
Ultra-processed foods aren’t automatically “evil,” but research suggests they can make it easy to eat more without noticing.
In a controlled NIH study, participants consumed about 500 extra calories per day on an ultra-processed diet compared with a minimally processed diet,
and gained weight during the ultra-processed phaseeven though meals were designed to be comparable in presented nutrients and calories.
This doesn’t mean every packaged food is a villain; it means food design and palatability matter.
3) Stress, sleep, and the “always-on” modern brain
Stress can influence eating patterns, hormones, and sleep. Sleep deprivation can disrupt hunger cues, lower energy for movement,
and increase cravings for quick energy. If your life feels like a notification storm, your metabolism doesn’t get a quiet workspace either.
4) Health conditions and medications
Some medical conditions (like hypothyroidism, polycystic ovary syndrome, or Cushing syndrome) and certain medications can contribute to weight gain.
That’s one reason obesity management in health care increasingly emphasizes individualized evaluation rather than one-size-fits-all advice.
5) Built environments: when “just go for a walk” isn’t realistic
Safe sidewalks, parks, lighting, and time matter. If your neighborhood lacks safe places to be activeor your schedule is so packed you’re basically
a human calendar reminderactivity becomes harder. Public health solutions often involve community design, not just personal motivation.
Health impacts: why the data matters (without scare tactics)
Cardiometabolic health
Obesity is associated with higher risk of conditions like type 2 diabetes, high blood pressure, and heart disease.
Risk doesn’t flip like a light switch at BMI 30, but on average, excess weight can raise the likelihood of these outcomesespecially when paired with
inactivity, poor sleep, or genetics.
Obesity and cancer risk
CDC reports that overweight and obesity are associated with increased risk of 13 types of cancer, and these cancers make up
about 40% of all cancers diagnosed in the U.S. each year. CDC also notes that in 2022, more than 716,000
obesity-associated cancers occurred in the United States. Not all of those cases are “caused” by obesity, but the association is strong enough that
maintaining a healthy weight is considered a meaningful prevention lever.
Costs: financial, medical, and emotional
Obesity carries major health system costs. CDC estimates obesity costs the U.S. health care system nearly $173 billion per year.
For children, CDC estimates annual medical costs of obesity around $1.3 billion (in 2019 dollars), and higher per-person costs for
children with obesity and severe obesity compared with children at a healthy weight.
And then there’s the cost you can’t always bill to insurance: stigma. Weight stigma can lead people to delay or avoid medical care, which can
worsen health outcomes. A health condition doesn’t get better when you’re afraid to be judged for having it.
Myths that won’t die (even though they really should)
Myth: “Obesity is just laziness.”
Fact: Obesity is influenced by many factorsgenes, environment, stress, sleep, medical conditions, medications, and access to healthy food and safe activity spaces.
“Just try harder” is not a public health strategy; it’s a slogan.
Myth: “If the scale goes down, health always goes up.”
Fact: Health is multi-dimensional. Improvements in fitness, blood pressure, glucose, sleep, and mental well-being can happen with or without large weight changes.
Weight can be one metric, but it’s not the only scoreboard.
Myth: “Kids just need stricter rules.”
Fact: For kids and teens, supportive routines work better than shame. Family meals when possible, consistent sleep schedules, more movement in fun forms,
and healthier default options tend to beat “food police” tactics. If a parent is worried about a child’s growth, a pediatric clinician can help guide next steps safely.
What actually helps: realistic prevention and support (no detox teas, no punishment workouts)
Make the healthy choice the easy choice
- Food access: affordable fruits/vegetables, healthier school meals, and less reliance on sugary beverages.
- Movement access: safe parks, sidewalks, school sports, and community programs that welcome all body sizes.
- Time access: predictable schedules and breaks (because “cook from scratch daily” isn’t realistic for every household).
Small shifts with big evidence behind them
Public health guidance often emphasizes dietary patterns over perfection. The Dietary Guidelines for Americans encourage limiting
added sugars and saturated fat (generally to less than 10% of daily calories for many age groups) and keeping sodium in check,
while focusing on nutrient-dense foods. You don’t need a personality transplant; you need repeatable habits.
Medical support is part of the picture
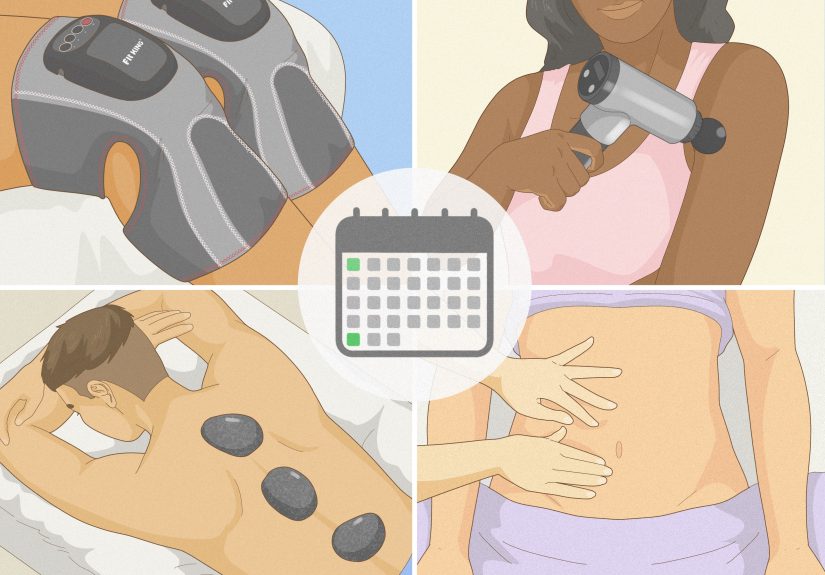
For some people, lifestyle changes alone aren’t enoughespecially with severe obesity or obesity-related complications. Evidence-based care can include
structured behavioral programs, medical nutrition therapy, medications, and sometimes surgeryalways guided by qualified clinicians and individual needs.
The “right” plan is the one that’s safe, sustainable, and improves health markersnot the one that wins internet points.
Where the story may be heading: the next chapter of obesity in America
The U.S. obesity conversation is shifting from “personal failure” to “chronic disease management,” and that matters.
It opens the door to better insurance coverage, more effective treatment options, and community-wide prevention strategies.
At the same time, access and equity remain major hurdles: healthier food, safe activity spaces, quality health care, and consistent preventive programs
are still unevenly distributed.
If there’s one takeaway from the obesity facts in America, it’s this: the numbers are big because the drivers are big. Fixing the problem requires
more than telling individuals to “do better.” It requires building a country where better is easier.
Experiences: what obesity can feel like in everyday American life (composite snapshots)
The facts are important, but they don’t always capture the lived reality. The experiences below are composite snapshotspatterns commonly reported by
patients, families, and communitieswritten to reflect the human side of obesity in America without pretending one story fits everyone.
1) The “time-poor household” experience
A lot of families aren’t choosing between kale and cupcakesthey’re choosing between “cook” and “sleep.” When you’re juggling work, school drop-offs,
caregiving, and a commute that feels like a side quest, dinner can become a rapid-fire decision: whatever is quick, affordable, and guaranteed to be eaten.
The irony is that convenience foods often cost more per nutrient, but less per minute. Over time, that tradeoff can nudge weight upward.
The household doesn’t need a lecture; it needs supportlike affordable groceries nearby, realistic meal ideas, and time to breathe.
2) The “desk job, tired brain” experience
Many adults describe gaining weight during years when life is most demandingcareer building, kids, stress, and chronic sleep shortage.
Sitting all day isn’t a character flaw; it’s how modern work is built. Add stress eating (because your nervous system wants comfort),
and you get a cycle: tired → less movement → more cravings → poorer sleep → repeat. People often say the hardest part isn’t “knowing what to do.”
It’s doing it when your schedule is packed tighter than a carry-on bag in an overhead bin.
3) The “food environment does the steering” experience
In some neighborhoods, the closest “grocery” is a convenience store where dinner is basically a shelf of snacks with excellent branding.
In others, safe walking paths and parks are limited, or it gets dark early and sidewalks aren’t friendly. When the environment makes healthier choices
inconvenient or unsafe, motivation can only carry you so far. People in these areas often become experts at improvising:
walking in malls, doing workouts at home, stretching during TV ads, buying frozen veggies because they last longer. The effort is therewhat’s missing is
consistent access.
4) The “doctor visit anxiety” experience
Weight stigma is real, and many people describe avoiding care because they expect judgment. They worry every symptom will be blamed on weight,
or that they’ll be talked to like a problem instead of a person. This can delay important screenings and treatment. When care is respectful,
outcomes improve: patients are more likely to come back, ask questions, and follow through. A surprisingly powerful “intervention” is simply
a health care setting that treats obesity as a medical conditionwithout sarcasm, shame, or assumptions.
5) The “teen perspective” experience
Teens often feel the pressure from every direction: social media, peers, sports, family, and the mirror.
Many describe wanting better energy and confidence but fearing that any change will be interpreted as “you weren’t good enough before.”
Supportive approaches focus on health and daily lifesleep, mood, stamina, strength, and enjoying movementrather than obsessing over the scale.
When adults model balanced habits and avoid negative talk about bodies, teens tend to feel safer seeking help. If a teen is concerned about weight or health,
involving a trusted clinician can keep the focus on safe, development-appropriate guidance.
These experiences underline a simple truth: obesity facts in America aren’t just statistics. They’re schedules, neighborhoods, school lunches,
stress levels, medical care experiences, and the constant friction of trying to be healthy in a world designed for convenience.
The most effective solutions respect that realityand aim to reduce the friction instead of blaming the person.