Table of Contents >> Show >> Hide
- A quick refresher: moles, “nevi,” and melanoma
- What the research suggests about fewer moles and more aggressive melanoma
- Why would fewer moles be linked with “more aggressive” melanoma?
- What “aggressive melanoma” really means (no scary movie soundtrack required)
- How to do smart skin checks when you don’t have many moles
- Prevention still matters, even if your skin seems “low-mole”
- Who should be extra cautious (yes, even with few moles)
- Bottom line: the “few moles” crowd still needs a plan
- Experiences people share about “few moles” and surprise melanoma (and what to learn from them)
If you’ve ever heard, “I don’t have many moles, so I’m probably fine,” I get it. It sounds logical.
Unfortunately, melanoma did not get the memo.
Here’s the twist: having lots of moles is a well-known risk factor for developing melanoma. But research has also found something
that feels downright unfairwhen melanoma shows up in people with fewer moles, it may be diagnosed at a thicker
(and potentially more dangerous) stage. That doesn’t mean “few moles = doomed.” It means “few moles = don’t get complacent.”
A quick refresher: moles, “nevi,” and melanoma
A “mole” (doctors often say nevus, plural nevi) is a common, usually harmless cluster of pigment-producing cells (melanocytes).
Most adults have at least a few. Some people have dozens. Some have hardly any. Your skin isn’t competing in a mole-count contestso no trophies either way.
Melanoma is a type of skin cancer that starts in melanocytes. It can appear as a changing mole, a new spot, or something that
doesn’t look like a mole at all (yes, really). The reason melanoma gets serious attention is that it can grow deeper into the skin and spread
if it isn’t caught early.
One important myth-buster: melanoma doesn’t always begin in a pre-existing mole. It can develop on “normal-looking” skin too. So if you’re scanning
your skin only for “my moles,” you may be missing the plot.
What the research suggests about fewer moles and more aggressive melanoma
Several studies have explored how mole count relates to the thickness of melanoma at diagnosis. Thickness matters because it’s one of the
strongest predictors of prognosis and helps determine staging and treatment.
The headline finding: fewer moles, thicker tumors (in some groups)
A widely cited analysis of U.S. patients looked at mole counts and melanoma thickness and found that many people diagnosed with melanoma had
relatively few moles. In that dataset, higher mole counts were associated with a greater likelihood of being diagnosed with a
thinner melanoma (especially in adults under 60), while people with fewer moles were more likely to have thicker melanoma at diagnosis.
Translation: high mole count can raise the odds of getting melanoma, but a low mole count doesn’t guarantee a “mild” case if melanoma occurs.
And it certainly doesn’t eliminate risk.
Two melanomas can behave like two different species
Researchers also discuss melanoma in terms of where it comes from:
nevus-associated melanoma (arising in a mole) versus de novo melanoma (arising on skin without a visible mole precursor).
Recent reviews and studies suggest nevus-associated melanomas are often diagnosed as thinner and show fewer aggressive features,
while de novo melanomas are more likely to be found thickerthough survival differences aren’t always clear-cut across studies.
Why would fewer moles be linked with “more aggressive” melanoma?
1) The vigilance gap (a.k.a. “It can’t be melanomaI don’t get moles”)
People with many moles often get labeled “high risk,” which can lead to more skin checks, more photos, and more conversations with dermatologists.
They may also be more likely to notice change because they’re already watching their skin like a hawk with a calendar reminder.
People with fewer moles may do fewer routine checks. The result can be delayed detectionmeaning the melanoma has more time to grow deeper.
Biology matters, but so does human nature.
2) The “doesn’t look like a mole” problem
Some of the most dangerous melanomas aren’t polite enough to follow the classic “ABCDE” script. Nodular melanoma, for example,
can grow more quickly, become thick sooner, and show up as a firm bump that may be dark, reddish, or even close to skin-colored.
Amelanotic melanoma can be pinkish or colorless, which makes it easier to dismiss as “a weird pimple” or “a stubborn spot.”
If you have few moles, you might not be looking for a new bump or pink patchbecause you’re expecting a dramatic, suspicious “mole.”
Melanoma is unfortunately fine with improvisation.
3) Different biology (nevus-associated vs. de novo)
Some research suggests melanomas that arise within moles may differ biologically from melanomas that arise de novo. In broad strokes,
nevus-associated melanomas are often found on the trunk and in younger patients and can be thinner at diagnosis, while de novo melanomas are
more often linked with older age and sun-damaged skin in certain locations (like head/neck).
That doesn’t mean “mole melanoma = harmless” or “de novo = hopeless.” It means there are multiple pathways to melanoma, and they don’t all show up
the same wayor on the same timeline.
4) Age and sun exposure can muddy the waters
Mole counts tend to change over a lifetime (many people have fewer visible moles as they age), and melanoma risk rises with cumulative UV exposure.
So “few moles” sometimes overlaps with “older” and “more sun history,” which can influence melanoma subtype and thickness at diagnosis.
What “aggressive melanoma” really means (no scary movie soundtrack required)
“Aggressive” can be a dramatic word, so let’s ground it. In medicine, clinicians look at specific features, including:
- Breslow thickness: how deep the melanoma extends into the skin (measured in millimeters).
- Ulceration: whether the surface skin is broken over the tumor (a higher-risk feature).
- Growth pattern and subtype: some subtypes (like nodular melanoma) may become thick sooner.
- Spread: whether there’s evidence it has moved to lymph nodes or other sites.
The key point for regular humans: thicker generally means more urgent. That’s why early detection is such a big dealand why
“I don’t have many moles” should never be your excuse to skip noticing new or changing spots.
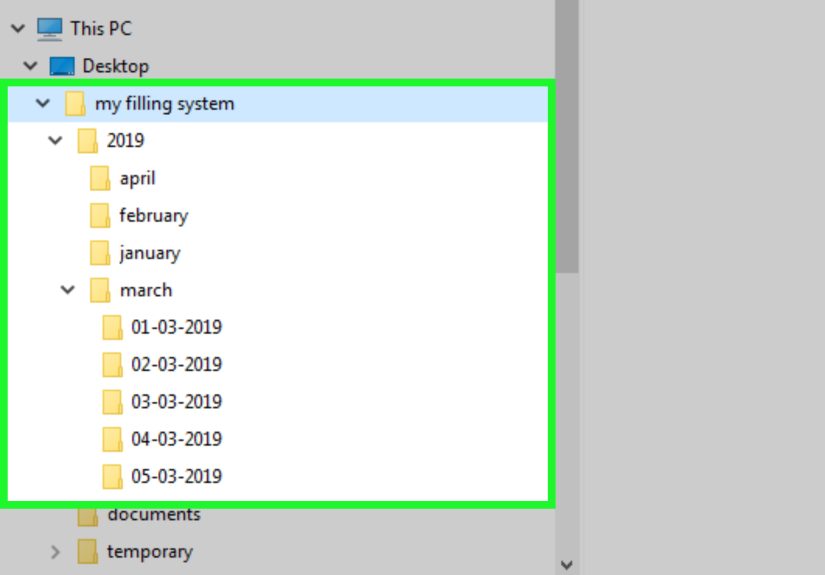
How to do smart skin checks when you don’t have many moles
The goal isn’t to become a full-time skin detective. The goal is to become familiar with your baseline so you can spot change.
Many experts recommend a monthly skin self-exam, especially if you have risk factors.
A simple, realistic monthly routine
- Use good light and a full-length mirror. Add a hand mirror for hard-to-see areas.
- Scan head to toe: scalp (part hair), ears, neck, chest, back, underarms, arms, hands, nails, legs, feet, soles.
- Don’t forget “sneaky spots”: between toes, under nails, buttocks, groin area.
- Look for NEW and CHANGINGnot just “weird-looking moles.”
- Consider photos (same lighting, same distance) if you’re monitoring a spot over time.
Use three tools: ABCDE, Ugly Duckling, and EFG
- ABCDE: Asymmetry, Border irregularity, Color variation, Diameter (often > 6 mm), Evolving (changing).
- Ugly Duckling: a spot that looks different from everything else on your body (even if it doesn’t “break” ABCDE).
- EFG (helpful for nodular melanoma): Elevated, Firm, and Growing (especially if it’s changing over weeks).
When to get a dermatologist involved
If you notice a spot that’s new and changing, growing quickly, bleeding without a good reason, not healing, or just “doesn’t belong,” it’s worth
getting checked. Dermatologists may use dermoscopy (a specialized magnifier/light) to evaluate patterns that the naked eye can’t see.
If needed, a biopsy is the only way to confirm diagnosis.
Prevention still matters, even if your skin seems “low-mole”
Melanoma risk is strongly linked to ultraviolet (UV) exposure. The most helpful prevention habits are boringbut boring is good when we’re talking about cancer:
- Seek shade, especially when UV is high.
- Wear protective clothing (long sleeves, wide-brim hat, UV-blocking sunglasses).
- Use broad-spectrum sunscreen and reapply as directed, especially when sweating or swimming.
- Avoid indoor tanning (your future self will thank you).
Think of sun protection like brushing your teeth: the payoff is mostly invisible, right up until it isn’t.
Who should be extra cautious (yes, even with few moles)
Mole count is only one piece of the melanoma risk puzzle. Other factors can raise risk, including:
- Personal or family history of melanoma
- Fair skin that burns easily, light eyes, red or blond hair, lots of freckles
- History of intense sunburns or heavy UV exposure
- Indoor tanning
- Many atypical (dysplastic) moles
- Weakened immune system (certain medical conditions or medications)
If you’re in a higher-risk group, ask a clinician what “reasonable monitoring” looks like for youbecause it can range from “keep up monthly checks”
to scheduled professional skin exams.
Bottom line: the “few moles” crowd still needs a plan
Here’s the cleanest way to hold this in your head without spiraling:
- Many moles can mean higher overall melanoma riskso watch for changes.
- Few moles does not mean low risk of serious melanomaso watch for new spots and fast change.
- Early detection usually means simpler treatment and better outcomes.
Melanoma prevention isn’t about fear. It’s about turning “I should probably check that” into “I checked thatdone.”
Required add-on: ~ of experiences
Experiences people share about “few moles” and surprise melanoma (and what to learn from them)
One of the most common experiences dermatology clinics hear is some version of: “I didn’t think it could be melanoma because I don’t really have moles.”
That belief can quietly shape what people pay attention to. If your skin has only a handful of moles, you may not feel like you have anything to monitorso
you’re less likely to do routine checks, less likely to take baseline photos, and more likely to give a new spot the benefit of the doubt.
Another frequently shared story is the “ordinary-looking bump” that didn’t set off alarms. Someone notices a firm, slightly raised spot on their arm or neck.
It isn’t jagged. It isn’t multicolored. It doesn’t scream ABCDE. It just… grows. Often, the person assumes it’s an ingrown hair, a bug bite, a stubborn pimple,
or a harmless skin tag. Weeks turn into months. When it finally gets checkedmaybe because it bleeds, becomes tender, or simply won’t go awayit turns out to be
a melanoma subtype that tends to grow downward faster than people expect. The lesson here isn’t “panic about every bump.” It’s “respect persistent growth.”
Many people also describe the emotional whiplash: they’ve heard public health messaging that focuses heavily on changing moles, so they feel blindsided when
a clinician says, “Melanoma doesn’t always start in a mole.” That’s a real mental reset. In practice, it means your skin check should include new
spots, non-healing areas, and colorless or pink lesionsespecially if they’re changing. People often say that once
they learn this, skin checks become less confusing because they stop trying to “grade” every spot and instead focus on the few that are new, evolving, or odd.
A different (but equally common) experience happens in families: a partner, parent, or close friend notices something on a hard-to-see areaback, scalp,
behind the earand insists it get checked. People sometimes joke about this (“fine, I’ll go to shut you up”), and then feel grateful later that someone else’s
eyes caught what theirs didn’t. This is why clinicians often recommend involving a buddy for back/scalp checks, especially if you live alone or you’re not
flexible enough to contort like a yoga instructor.
Finally, there’s the experience of relief that comes from a quick evaluation. Many “scary-looking” spots turn out to be benign, and many “meh-looking” spots
deserve a closer look. People often report that the biggest benefit of building a simple habitmonthly checks, a couple of photos, and prompt evaluation when
something changesisn’t just medical. It’s psychological. You replace vague worry with a concrete plan. And when it comes to melanoma, a plan is powerful:
it helps you catch problems earlier, when treatment tends to be more straightforward.