Table of Contents >> Show >> Hide
- What Scabies Is (And Why It Feels So Personal)
- “Scabies Bites” vs. Bug Bites: The Key Differences
- What Scabies Rash Can Look Like
- A Practical Self-Check: Does This Sound Like Scabies?
- Scabies Look-Alikes (And How to Tell Them Apart)
- How Doctors Confirm Scabies
- What to Do If You Think It’s Scabies
- When Scabies Needs Faster Medical Attention
- Experiences People Commonly Share (500+ Words)
If you’ve been Googling “scabies bites,” you’re not alone. The confusing part is that scabies isn’t really a
biteit’s an itchy skin reaction caused by tiny mites that burrow into the top layer of skin and set off an
allergy-like response. The result can look like bug bites, pimples, or hives… and it can drive you absolutely
bananas, especially at night.
This guide breaks down how to identify scabies (without turning your bathroom mirror into a crime lab), what
scabies commonly looks like on different body areas, and how to tell it apart from bed bugs, eczema, and other
itchy imposters.
What Scabies Is (And Why It Feels So Personal)
Scabies is a contagious skin infestation caused by the human itch mite (Sarcoptes scabiei). The mite burrows
into the skin to live and lay eggs. Your body reacts to the mites and their debris, which leads to intense itching
and a rash. The itching is classically worse at night, which is rude, but very typical.
Scabies usually spreads through prolonged skin-to-skin contact (including sexual contact). It can also spread
sometimes by sharing bedding, towels, or clothingespecially in crowded settings or when someone has
crusted scabies (a more severe form with many more mites).
Quick myth-buster: Can you get scabies from pets?
Pets don’t spread human scabies. Animals can have a different type of mite (mange) that may cause temporary
itching in people, but it doesn’t survive or reproduce on humans the way human scabies does.
“Scabies Bites” vs. Bug Bites: The Key Differences
Many rashes can look like bites. What makes scabies different is the pattern, the timing,
and the company it keeps (meaning: other people around you start itching too).
-
Itching is intense and often worse at night. If you’re fine all day but become a scratching gremlin
at bedtime, scabies moves higher on the list. -
The rash often shows up in classic “scabies zones.” Think finger webs, wrists, elbows, armpits,
waistline, buttocks, nipples, and genitals. - Burrows may be present. These are tiny, thin linessometimes wavy or S-shapedwhere the mite has tunneled.
-
Symptoms can be delayed. After a first exposure, symptoms often take weeks to appear. If you’ve had
scabies before, symptoms can show up much faster after re-exposure.
What Scabies Rash Can Look Like
Scabies doesn’t have one perfect “poster child” look. Depending on your skin tone and how long it’s been going on,
it may appear as small red or brown bumps, tiny blisters, hive-like patches, or scratch marks. Sometimes it appears
in lines or clusters and can resemble insect bites.
1) The itch pattern: the midnight signature
The most common scabies symptom is intense itching that tends to be worse at night. Itching can be
severe enough to interrupt sleep. Scratching can also cause sores, which may later become irritated or infected.
2) Burrows: the “tiny pencil mark” clue
Burrows can look like very thin grayish, whitish, or skin-colored linessometimes slightly raised. They’re easiest
to spot in areas with thinner skin, like between the fingers or on the wrists. Not everyone can see them, and you
don’t need visible burrows to have scabiesbut if you do see them, they’re a strong clue.
3) Common locations in adults and teens
Scabies often shows up in these areas:
- Between the fingers
- Wrists and elbows (especially skin folds)
- Armpits
- Waistline and belly button area
- Buttocks
- Nipples/areola area
- Genitals (penis/scrotum or vulvar area)
4) Common locations in babies and young kids
In infants and young children, scabies can be more widespread and may involve the scalp, face, neck, palms, and soles.
That difference mattersbecause what looks “unusual” in adults can be typical in little kids.
A Practical Self-Check: Does This Sound Like Scabies?
This is not a diagnosis (only a clinician can diagnose scabies), but it can help you decide whether to get checked.
Scabies becomes more likely if you can answer “yes” to several of these:
- The itch is worse at night and has lasted more than a few days.
- The rash is in classic scabies areas (finger webs, wrists, armpits, waist, buttocks, genitals).
- Someone close to you is also itchy (household members, partner, dorm roommate).
- You had close skin-to-skin contact with someone who had an unexplained itchy rash.
- Over-the-counter anti-itch creams help temporarily but the itch keeps coming back.
- You notice thin lines/burrows or a line-like rash pattern in addition to bumps.
Scabies Look-Alikes (And How to Tell Them Apart)
Bed bugs
Bed bug bites often show up on exposed skin (arms, shoulders, face, neck) and may appear in clusters or lines.
Scabies more often targets skin folds and “hidden” areas like finger webs and the waistline. If the rash mainly
appears after sleeping and is on exposed areas, bed bugs are a strong contender.
Fleas or mosquitoes
Flea bites often cluster around ankles and lower legs. Mosquito bites tend to be isolated, raised welts on exposed
skin. Scabies usually causes ongoing itching and a rash pattern that spreads in classic zones, often with worsening
nighttime itch.
Eczema or contact dermatitis
Eczema can be intensely itchy and may flare with dry air, soaps, stress, or allergens. Contact dermatitis often
appears where a trigger touched the skin (new detergent, fragrance, jewelry metal). Unlike scabies, these conditions
are not contagiousso the “my whole household is itchy now” clue points away from eczema and toward scabies.
Hives
Hives are raised, smooth, and often move around or change shape within hours. Scabies bumps tend to persist and are
often accompanied by scratch marks and a predictable distribution pattern.
Folliculitis
Folliculitis is inflammation or infection of hair follicles, commonly appearing as pimple-like bumps centered on
hair follicles, sometimes with tenderness. Scabies can look “pimply,” but the location pattern (finger webs, wrists,
waistline) and night itch are the clues that separate them.
How Doctors Confirm Scabies
Clinicians often diagnose scabies by examining the rash pattern and asking about itching (especially nighttime),
exposure history, and whether others in the home are affected. If the diagnosis isn’t clear, they may use:
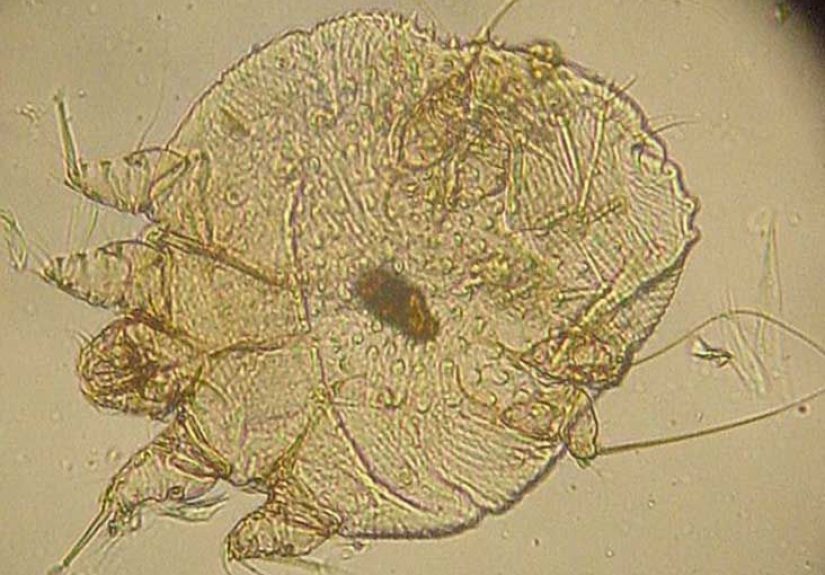
- Skin scraping to look for mites, eggs, or mite debris under a microscope
- Dermoscopy (a handheld magnifier) to spot features consistent with burrows and mites
- Adhesive tape test (in some settings) to collect material from the skin surface
Important: a negative scraping doesn’t always rule it out. Scabies mites can be few in number in typical cases, so
clinicians combine testing with the overall clinical picture.
What to Do If You Think It’s Scabies
Scabies is treatable, but it usually requires prescription medication. If you suspect scabies, it’s smart to get
checkedespecially if the itch is severe, you’re losing sleep, or multiple people around you are itchy.
Common treatments (your clinician will choose what fits you)
-
Permethrin 5% cream is a common first-line treatment. It’s applied to the skin as directed and
may be repeated about a week later, depending on instructions. - Oral ivermectin is sometimes used, including in certain outbreaks or harder-to-treat cases.
Do not self-prescribe or borrow scabies medication. Correct dosing and timing matters, and certain groups (like
young children, pregnant people, or those with medical conditions) need personalized guidance.
Treat close contacts at the same time
One of the biggest reasons scabies keeps circling back is that only one person is treated. Many public health and
dermatology recommendations stress treating household members and close contacts at the same time to stop the
“ping-pong” effect.
Clean smart, not frantic
You don’t need to disinfect your life down to the last throw pillow seambut you should handle items that recently
touched skin. Common guidance includes:
- Wash clothing, bedding, and towels used in the 3 days before treatment using hot water and a hot dryer cycle.
- If an item can’t be washed, seal it in a plastic bag for several days (often at least 72 hours) up to a week.
- Vacuum carpets and upholstered furniture the day you start treatment.
Why you might still itch after treatment
Even after successful treatment, itching can continue for a couple of weeks because your skin is still calming down
from the allergic reaction. However, if new burrows or new bumps keep appearing, follow upretreatment may be needed.
When Scabies Needs Faster Medical Attention
Get medical care promptly if:
- You suspect scabies in a baby or young child (distribution and treatment approach can differ).
- You’re immunocompromised or have widespread thick crusting that could suggest crusted scabies.
- The skin becomes very painful, swollen, warm, or oozing (possible secondary infection).
- The rash is rapidly worsening or you have fever or feel unwell.
Experiences People Commonly Share (500+ Words)
Because scabies can look like so many things, a lot of people don’t recognize it right away. Below are examples of
experiences that clinics, school nurses, and households commonly describe. These are composite scenarios meant to
feel familiarnot a substitute for medical advice.
1) “Why is it always worse at night?”
A very common story starts with sleep getting wrecked. During the day, you’re distractedwork, school, errands,
scrolling, life. Then night hits and suddenly your skin feels like it’s auditioning to be a percussion instrument.
People often describe the itch as “deep,” “relentless,” or “impossible to ignore.” They try a new body wash, switch
detergents, change sheets twice, and buy an over-the-counter anti-itch cream that works for about 45 minutes… then
the itch returns like it pays rent.
The clue that often pushes them toward scabies is that the itch isn’t random: it keeps targeting the same zones
(wrists, finger webs, waistline), and it escalates at night. When someone finally sees a clinician, the rash pattern
plus the night itch becomes the big “aha.”
2) The household domino effect
Another classic experience: one person itches first. A week or two later, a partner starts scratching. Then a child
says, “My hands itch.” Then everyone is staring at their skin under bright bathroom lighting like they’re reading
fine print on a contract.
This is where scabies really reveals itself as a team sport (unfortunately). People often assume, “If I treat me,
I’m done.” But scabies can spread through close contact, so households sometimes get reinfected unless close
contacts are treated at the same time. Families often describe a “second wave” of itching after the first person
finished treatmentusually because someone else was silently infested or treatment timing didn’t line up.
The emotional side is real, too. People worry it means they’re “dirty,” but scabies has nothing to do with hygiene.
It’s about exposure and contact. Once families understand that, the stress level drops and the plan becomes simpler:
treat everyone appropriately, wash recent linens, and stop the cycle.
3) “I thought it was bed bugs… until the rash didn’t match.”
Bed bugs get blamed early because it sounds logical: itchy rash + sleep = bed bugs. Many people even go into full
detective modechecking mattress seams, buying traps, cleaning like they’re prepping for a TV makeover.
The twist comes when the rash keeps showing up in areas bed bugs don’t “prefer,” like between the fingers, around
wrists, and in skin folds. Or when there’s little evidence of bed bugs in the environment. When someone learns that
scabies can look like bites and even appear in lines, it suddenly makes sense why the rash kept “hiding” in those
classic scabies spots instead of staying mostly on exposed skin.
4) The post-treatment “Did it work?” phase
Even after treatment, many people go through a frustrating period of lingering itch. They assume treatment failed,
but in many cases, the skin is still reacting to the earlier infestation. People often describe it as a “phantom
itch” that improves gradually rather than instantly. This is why follow-up guidance matters: watch for truly new
burrows or fresh bumps that continue appearing, and check in with a clinician if symptoms persist beyond the window
you were told to expect.
The big takeaway from these experiences is simple: scabies is common, treatable, and often misidentified at first.
If the itch is intense (especially at night), the rash is in classic scabies zones, and others around you are
itching too, it’s worth getting evaluated sooner rather than later.