Table of Contents >> Show >> Hide
- What changed: from “no” to “case-by-case”
- Airline pilot basics: why the medical certificate matters
- The FAA pathway for insulin-treated diabetes
- What “safe” diabetes management looks like in aviation terms
- Reality check: the challenges are real (and manageable)
- Step-by-step mindset: how to approach the goal strategically
- Common questions (the ones people whisper in hangars)
- Bottom line: yes, it’s possibleand it’s a professional-level commitment
- Experiences from pilots and trainees with T1D (extra 500+ words)
For decades, “airline pilot” and “type 1 diabetes” sounded like two labels that couldn’t share the same name tag.
Not because people with T1D aren’t capable (they are), but because aviation medicine is obsessed with one thing:
predictability. And diabetesespecially insulin-treated diabeteswas historically viewed as too risky because of
the possibility of sudden low blood sugar (hypoglycemia) during flight.
Here’s the modern plot twist: the FAA now has a pathway for insulin-treated diabetes mellitus (ITDM) applicants to be
considered for first- and second-class medical certification through the special issuance process, using a
risk-assessment protocol built around today’s toolsespecially continuous glucose monitoring (CGM).
Translation: a well-managed, well-documented type 1 diabetes diagnosis is no longer an automatic “dream grounded.”
This article explains what changed, what the FAA is actually looking for, how pilots with T1D manage glucose in real cockpit life,
and how to think strategically about training and career planningwithout sugarcoating the paperwork (because the paperwork does not deserve kindness).
What changed: from “no” to “case-by-case”
The FAA has long used special issuance authority to consider certain medical conditions that are technically disqualifying under standard rules.
For insulin-treated diabetes, third-class pathways existed earlier (with strict monitoring), but the big shift arrived in 2019:
the FAA announced a protocol that makes it possible to consider first- and second-class special issuance for a subset of low-risk applicants.
That matters because first-class is the medical certificate typically needed for airline transport pilot privileges.
The reason this became possible isn’t magicit’s data. Modern diabetes management provides more visibility than ever:
CGMs, improved meters, better insulin analogs, and pumps can reduce both the frequency and severity of dangerous glucose swings.
Aviation regulators care less about your diagnosis label and more about your demonstrated stability and your risk mitigation plan.
Airline pilot basics: why the medical certificate matters
Becoming an airline pilot isn’t just “learn to fly, apply to airlines, collect tiny bags of pretzels as tribute.”
Your medical certificate class shapes what you can do professionally:
- First-class medical: typically required to exercise airline transport pilot privileges (common for airline careers).
- Second-class medical: typically tied to commercial pilot privileges (many paid flying roles, not always airlines).
- Third-class medical: generally associated with private pilot privileges and some limited scenarios.
With type 1 diabetes, the pathway (for any class) is generally through special issuancemeaning the FAA reviews your case and decides
whether you can safely exercise the privileges of the certificate you’re requesting.
The FAA pathway for insulin-treated diabetes
If you want airline flying with T1D, the key phrase you’ll hear is: “Insulin-Treated Diabetes Mellitus (ITDM) protocol.”
In plain English, the FAA wants proof that:
- You’ve been clinically stable on your current regimen (often described as a minimum stable period).
- Your day-to-day management shows low risk of sudden incapacitation, especially from severe hypoglycemia.
- You’re under appropriate medical care and you’re tracking the right data over time.
- You can follow a monitoring plan consistentlybecause aviation is allergic to “I’ll wing it.”
CGM is a big deal (especially for first/second class)
For first- and second-class consideration under the modern protocol, CGM data is central because it provides continuous, time-stamped evidence:
not just a handful of “good” readings, but the full storyovernights, workdays, stress days, normal days, days when your body decides it’s a mystery novel.
The FAA’s goal is not to punish you with spreadsheets (though it can feel that way). It’s to evaluate whether your real-world glucose pattern
shows good control and a low likelihood of dangerous lows during critical phases of flight.
Expect comprehensive documentation
Special issuance for ITDM is documentation-heavy by design. Think of it like proving you’re safe to operate a complex system while managing another complex system.
Your submission package commonly includes:
- Treatment history, regimen details, and evidence of stability over time.
- CGM data covering a meaningful period (the protocol emphasizes having a track record, not a highlight reel).
- Laboratory results and clinician reports that reflect overall management.
- Complications screening (because long-term risks like cardiovascular or eye complications matter for aviation safety).
- Evidence of hypoglycemia awareness and how you prevent/treat lows.
The FAA’s medical logic is straightforward: low blood sugar can impair thinking, coordination, speech, and vision; severe hypoglycemia can cause seizures
or loss of consciousness. In aviation, that’s not “oops,” that’s “we don’t do that here.”
What “safe” diabetes management looks like in aviation terms
Diabetes management for flight isn’t about being perfect. It’s about being predictable, prepared, and honest with your data.
The safest pilots with T1D typically operate with layered defenseslike aviation itself.
Layer 1: A stable baseline
Stability matters more than heroic effort. If your glucose is swinging wildly, you’re spending your attention budget on constant corrections.
In flight training and airline ops, attention is a finite resourcespend it on flying, not on emergency snack negotiations with your pancreas.
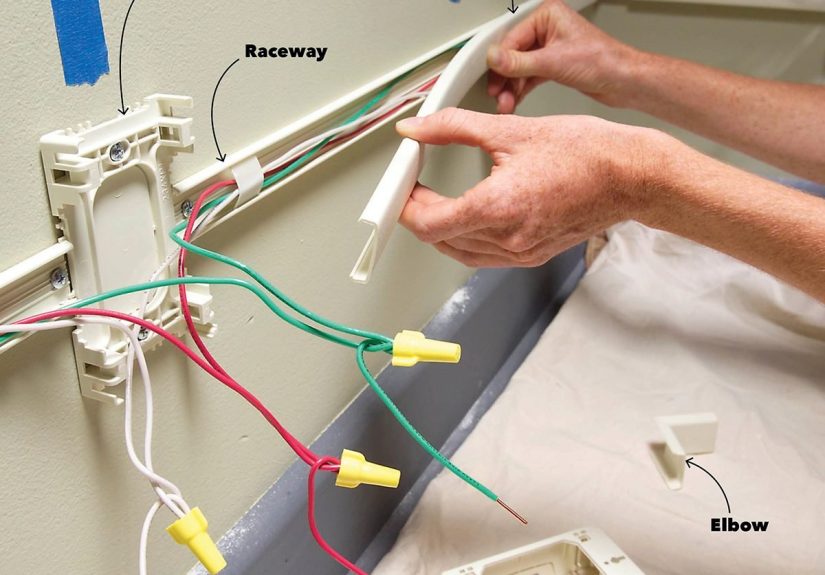
Layer 2: Continuous monitoring (and realistic backup plans)
CGMs are powerful, but no technology is perfect 100% of the time. Sensors can fail, compress, read inaccurately, or lag behind blood glucose changes.
Good aviation practice is redundancy: pilots commonly carry a fingerstick meter and supplies as a backup, plus extra sensor supplies when appropriate.
Layer 3: Preventing and treating lows quickly
Hypoglycemia can start with shakiness, sweating, hunger, or irritabilityand can progress to confusion or impaired coordination if untreated.
Severe lows can become dangerous fast. That’s why pilots with diabetes typically plan for early detection and rapid treatment.
A standard public-health approach to treating lows is the “15-15 rule” (fast carbs, wait, recheck), though your personal diabetes plan should be tailored with your clinician.
In practical cockpit terms: fast-acting carbs are not optional. They are as essential as a flashlight in a dark cockpit.
(And unlike a flashlight, glucose tablets won’t roll under the seat and vanish into the aircraft’s secret alternate dimension quite as easily.)
Layer 4: A “no-surprises” mindset
Aviation loves checklists because humans are excellent at being confident and wrong at the same time.
Many pilots with T1D use structured routines:
- Pre-flight planning that includes meals, timing, and glucose trend awareness.
- Conservative targets (with clinician guidance) to reduce the chance of dropping low during high workload phases.
- Alarm settings that prioritize early warning rather than late drama.
- Clear rules for when to pause, treat, and stabilizewithout ego.
Reality check: the challenges are real (and manageable)
Airline life is not a steady 9-to-5 with guaranteed lunch at noon. Diabetes loves routine; airlines love schedule changes.
Here are the common friction pointsand what successful pilots do about them.
1) Irregular schedules and time zones
Changing duty times can affect sleep, stress hormones, meal timing, and insulin sensitivity. Many pilots compensate by keeping management simple and repeatable:
predictable meal options, careful dosing strategies, and conservative “guardrails” around high-risk time windows.
2) Stress and adrenaline
Stress can push glucose up for some people, while sudden exertion or long gaps between meals can push it down.
The trick is not to guessit’s to watch the trend and respond early.
3) Access to food and breaks
In training aircraft and airline ops alike, there are phases where you’re busy and you can’t just casually host a snack buffet.
Many pilots pack compact, predictable options: fast carbs for lows, and slower carbs/protein for stability.
4) Medical documentation as an ongoing job
Special issuance isn’t a one-and-done trophy you place on a shelf. It often involves periodic follow-ups and updated data submissions.
The pilots who do best treat documentation like logbooks: boring, necessary, and oddly satisfying when done right.
Step-by-step mindset: how to approach the goal strategically
Without turning this into a legal checklist (because requirements can evolve), here’s a practical strategy that aligns with how the FAA thinks:
Start with an Aviation Medical Examiner (AME) who understands the process
Not every AME is equally familiar with ITDM special issuance pathways. A knowledgeable AME can help you understand what documentation typically matters,
what common gaps delay decisions, and how to present your case clearly and accurately.
Build a “medical portfolio” early
If your goal is the airlines, don’t wait until you’re ready to apply to start organizing your diabetes records.
Keep consistent reports, clinician notes, and trend data. A strong application is usually less about dramatic improvement and more about consistent proof of stability.
Train like a professional, not like a gambler
Aviation is risk management. Your diabetes routine should mirror that culture:
predictable habits, conservative buffers, redundancy, and a willingness to pause and fix a problem early rather than “push through.”
Common questions (the ones people whisper in hangars)
“Will I definitely be approved?”
No one can promise approval. Special issuance is case-by-case. But “case-by-case” is a door,
and that door did not exist in the same way for airline-level privileges before modern protocols.
“Do I have to be ‘perfect’?”
The goal is not perfection; it’s safety and reliability. Regulators and clinicians know that real life exists.
What matters is your risk profileespecially your history with severe hypoglycemia, your awareness of lows, and your ability to manage trends consistently.
“Does technology make it easier?”
Technology helps because it creates data and early warnings. But the FAA isn’t certifying your CGMit’s evaluating you using the data your tools provide.
Think of CGM and pumps as part of a larger system: training, routines, planning, and backup procedures.
Bottom line: yes, it’s possibleand it’s a professional-level commitment
Becoming an airline pilot with type 1 diabetes is no longer a fantasy reserved for inspirational posters.
It’s a real pathwayone that rewards strong management, careful documentation, and a safety-first mindset.
If you’ve already learned to count carbs, correct highs, prevent lows, and keep showing up day after day,
you’ve already been training in a discipline aviation respects: operating calmly in a world that does not always cooperate.
Add flight training, add paperwork, add checklists, and yesadd snacks. You’ve got this.
Experiences from pilots and trainees with T1D (extra 500+ words)
The most useful advice often comes from the lived routinethe tiny decisions that don’t look heroic but keep everything safe.
Below are composite experiences based on common themes shared by pilots and trainees navigating the FAA process and cockpit life with type 1 diabetes.
Names and details are generalized, but the strategies are very real.
Experience #1: “I treated my CGM like a co-pilot, not a crystal ball.”
One regional first officer described the biggest mindset shift as learning to stop “reacting late.”
Before flying professionally, they sometimes waited until they felt low to treatfine for everyday life, not fine for a flight deck.
Their solution was boringly effective: alarms set earlier, a habit of checking trends before high-workload phases,
and a strict rule that fast carbs live in the same spot every time (so they’re never hunting through a bag like it’s a scavenger hunt).
They also carried a backup meter and supplies even though their CGM was usually accurate.
“In aviation,” they said, “you don’t bet the flight on one system.”
What surprised them most wasn’t the flyingit was the documentation cadence. They built a monthly routine:
export reports, file them, and keep clinician notes organized. “It’s like logging flight hours,” they joked.
“Nobody does it for fun, but everyone regrets skipping it.”
Experience #2: “Time zones made my body weird, so I made my plan simpler.”
A cargo pilot who frequently crossed time zones said the hardest part wasn’t the clock changeit was the second-order effects:
sleep disruption, inconsistent meal timing, and stress hormones making glucose behave like it had a personality.
Their strategy was simplicity and predictability: repeatable meal choices when possible, conservative dosing adjustments under clinician guidance,
and an emphasis on stable ranges rather than chasing “perfect” numbers mid-duty.
They also learned to treat fatigue like a diabetes variable, not just a nuisance.
Poor sleep made it harder to notice subtle symptoms and easier to miss trend shifts.
So they built “micro-checks” into their routine: quick trend glance at defined moments, then back to flying.
The goal wasn’t to obsess; it was to prevent surprises.
Experience #3: “Flight training taught me that workload matters as much as glucose.”
A student pilot working toward commercial training described the early days as a juggling act:
learning maneuvers, radios, navigation, weather, and the uncomfortable reality that your brain is also a glucose-powered device.
They noticed that intense training blocks could nudge glucose downwardpartly from adrenaline, partly from the physical effort of training days,
and partly from long gaps between meals.
Their instructor (not a medical professional, just an excellent safety nerd) encouraged a simple approach:
plan snacks like you plan fuel reserves, and address issues early.
Over time, the student built confidence by practicing responses on the ground:
recognizing early low symptoms, knowing exactly what “15 grams” looks like in their chosen snacks,
and keeping a consistent pre-flight routine that included a trend check.
The student said the emotional win wasn’t just “I can fly.” It was “I can fly consistently.”
They also learned the value of communication without oversharing.
In training, they didn’t dramatize diabetes, but they were clear about safety steps:
“If I need a minute to treat a low, I’ll say so.” That professionalismcalm, direct, solutions-orientedis exactly what aviation culture wants.
Across these experiences, the common thread is confidence built from systems: CGM plus backup, routines plus flexibility,
early action instead of late panic, and documentation treated like part of the job.
For the right candidate, type 1 diabetes isn’t an automatic career enderit’s a reason to become exceptionally good at risk management.
And honestly, that’s kind of the whole pilot job anyway.